VA Mental Health: Additional Action Needed to Assess Rural Veterans' Access to Intensive Care
Fast Facts
Our past work and other research shows that veterans—especially those living in rural areas—can have trouble getting the mental health care they need.
Veterans Health Administration officials confirmed that veterans living in rural areas face unique barriers to accessing mental health care, such as staff shortages in rural facilities and transportation issues.
VHA assesses its intensive mental health care programs but doesn't specifically monitor rural veterans' access. Our review of VHA's service use data found differences between rural and urban areas.
We recommended ways for VHA to help ensure these programs effectively serve rural veterans.

Highlights
What GAO Found
The Veterans Health Administration (VHA) provides intensive mental health care for veterans with serious mental illness—disorders resulting in serious function impairment, such as schizophrenia or bipolar disorder. To monitor veterans' access to its inpatient, residential, and outpatient intensive mental health care programs, VHA analyzes the extent to which veterans use these programs. It also analyzes performance data, such as how long veterans wait for residential care and the ratio of patients to program staff. However, VHA does not analyze its data by rurality to compare program utilization and performance for veterans living in rural areas with those living in urban areas. Doing so would help VHA understand the extent to which programs effectively reach rural veterans.
In analyzing VHA's fiscal year 2021 data, GAO found rural veterans used intensive mental health care programs at lower rates than their urban counterparts. For example, the rate at which rural veterans used outpatient care was approximately 21 percent, compared with a utilization rate of 79 percent for urban veterans (see figure). VHA data show 27 percent of veterans with serious mental illness who received VHA care lived in a rural area in the same year. According to VHA officials, there may be various reasons rural veterans use care less than urban veterans, such as other demographic differences.
Proportion of Rural and Urban Veterans Using VHA Intensive Mental Health Care, Fiscal Year 2021
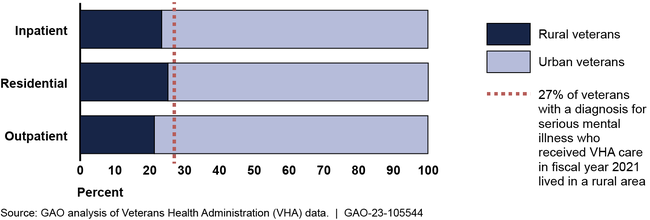
Note: Inpatient programs, such as a hospital stay, are for veterans experiencing acute mental health crisis. Residential programs provide residential and treatment services. Outpatient programs provide treatment services to veterans. GAO uses the term “rural veteran” to include veterans living in rural, highly rural, and insular island areas.
In 2021, VHA updated its guidelines for establishing inpatient and residential intensive mental health care programs to account for projected demand and geographic data, such as the location of where veterans live. However, guidelines for its outpatient intensive mental health care programs do not account for where veterans live. For example, guidelines for establishing rural-focused programs “strongly encourage” establishment in rural areas but do not otherwise identify parameters facilities should use in doing so, such as where veterans live or drive times for reaching a facility. Assessing and updating, as appropriate, its guidelines for establishing outpatient programs to include such parameters would be consistent with the Department of Veterans Affairs' goals of improving access to care for rural veterans and veterans with serious mental illness.
Why GAO Did This Study
Serious mental illness is a persistent and growing concern for our nation's veterans. Research shows veterans with serious mental illness who live in rural areas can face challenges accessing this care, such as long drive times to facilities.
The Sgt. Ketchum Rural Veterans Mental Health Act of 2021 included a provision for GAO to study the intensive mental health care that VHA makes available to rural veterans. Among other objectives, this report examines the information VHA uses to monitor access to such care, what these data show about rural veterans' access, and the guidelines VHA uses to establish programs for rural veterans.
GAO reviewed VHA documentation and policies on its intensive mental health care programs and fiscal year 2021 data (most recent available) on utilization and performance for these programs. GAO also interviewed VHA officials and officials from three health care systems selected for geographic and program variation.
Recommendations
GAO is making four recommendations, including that VHA analyze intensive mental health care utilization and performance data by rurality and assess and update, as appropriate, guidelines for establishing outpatient intensive mental health programs. The Department of Veterans Affairs concurred with the recommendations and identified steps it would take to implement them.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Veterans Health Administration | The Department of Veterans Affairs Under Secretary of Health should ensure that the Office of Mental Health and Suicide Prevention analyzes, by rurality, the utilization and performance data it uses to monitor access to intensive mental health care and include such analyses in program performance assessments. (Recommendation 1) |
VHA concurred with our recommendation and has taken steps to implement it. As of March 2024, VHA developed and deployed to Office of Mental Health and Suicide Prevention employees a dashboard to support intensive mental health care programs with investigating potential differences in quality measures stratified by vulnerable demographic groups, such as rurality. The Office of Mental Health and Suicide Prevention also completed analyses by rurality of patient utilization and performance data it uses to monitor access for its intensive mental health care programs. Specifically, for its outpatient intensive mental health care programs, the office analyzed program utilization and outcomes by rurality; for its residential intensive mental health care programs the agency incorporated rurality into its analyses of wait-times for and admissions to care; and for its inpatient intensive mental health care programs the agency examined admission rates by rurality. VHA also incorporated rurality from these analyses into annual program evaluations for outpatient and residential intensive mental health care program, according to agency documents. These actions fulfill the intent of the recommendation and as such, we are closing this recommendation as implemented.
|
| Veterans Health Administration | The Department of Veterans Affairs Under Secretary of Health should ensure that the Office of Mental Health and Suicide Prevention incorporates into its monitoring efforts, as appropriate, analysis of referral and claims data for intensive mental health care services provided through community care. (Recommendation 2) |
VHA concurred with our recommendation and has taken steps to implement it. As of December 2023, the Office of Mental Health and Suicide Prevention has worked with the Office of Integrated Veteran Care to develop business rules and a methodology to integrate community care data into monitoring efforts for residential and other intensive mental health care services. Specifically, the offices created rules for extracting data necessary to integrate community care data into monitoring efforts for mental health residential treatment to include information on referrals, claims, episodes of cares, bed days of care, and wait times by demographic variables, such as rurality, into regular recurring reports. The office revised the methodology to apply it to other intensive mental health care services provided in the community. These actions fulfill the intent of the recommendation and as such, we are closing this recommendation as implemented.
|
| Veterans Health Administration | The Department of Veterans Affairs Under Secretary of Health should assess and update, as appropriate, its guidelines for establishing outpatient intensive mental health care programs to incorporate parameters to factor in where veterans in need live. (Recommendation 3) |
VHA concurred with our recommendation and has taken steps to implement it. As of December 2023, the Office of Mental Health and Suicide Prevention had developed a data tool and a quick reference document to provide guidance to VHA facilities to use and inform treatment and programming needs of veterans in more rural counties. The data tool allows facilities to examine by rurality measures like the percentage of veterans with a diagnosis relevant to VHA intensive outpatient programs that are being served by such programs in a given area-where veterans in need live. According to VHA, the tool and reference document, which provides instruction on how to use the tool to examine demographic differences to understand access to care, provide guidance to facilities for decision making. VHA reported that the Office of Mental Health and Suicide Prevention provided information to VHA field staff on assessing rural veteran's access to intensive mental health care, including using the tool. These actions fulfill the intent of the recommendation and as such, we are closing this recommendation as implemented.
|
| Veterans Health Administration | The Department of Veterans Affairs Under Secretary of Health should update its guidelines for providing seed funding to Rural Access Network for Growth Enhancement or Enhanced Rural Access Network for Growth Enhancement programs to include data on the locations of veterans with serious mental illness. (Recommendation 4) |
VHA concurred with our recommendation and has taken steps to implement it. At the time of our review, the applications for seed funding for Rural Access Network for Growth Enhancement or Enhanced Rural Access Network for Growth Enhancement programs required information on rurality of zip codes served by the proposed program. The Office of Mental Health and Suicide prevention selected for funding only programs proposing to serve areas in which 90 percent of veterans live in rural areas. According to office officials, the agency assumed rather than requested information on the prevalence of serious mental illness-the population meant to be served by the intensive mental health care programs-among veterans served in the application areas. As of April 2024, VHA updated the funding application conditions for Rural Access Network for Growth Enhancement or Enhanced Rural Access Network for Growth Enhancement programs to target veterans with serious mental illness and that live in rural areas. These actions fulfill the intent of the recommendation and as such, we are closing this recommendation as implemented.
|
