Veterans Health Care: Staffing Challenges Persist for Fully Integrating Mental Health and Primary Care Services
Fast Facts
With the growing demand for mental health services, Veterans Health Administration facilities must make providers—like psychologists and psychiatrists—available within primary care settings to assess and treat veterans with mild-to-moderate symptoms and conditions, like anxiety or depression.
But persistent staffing issues at some VHA facilities have negatively affected efforts to integrate these services into primary care settings. To address this, some facilities have offered flexible work schedules and provided more technology to reduce workloads. We recommended that VHA evaluate these and other mitigation strategies.

Highlights
What GAO Found
The Veterans Health Administration (VHA) requires its medical facilities serving at least 5,000 veterans annually to integrate mental health services into the primary care services they provide. Specifically, facilities are required to have mental health providers, such as psychologists, psychiatrists, and social workers, available within primary care settings to work collaboratively and share responsibility with primary care providers to (1) assess and treat veterans with mental health symptoms and conditions, such as anxiety or depression; and (2) follow up with those veterans to monitor symptoms and adherence to medications, and provide education and referral services.
VHA data show that as of February 2022, about 79 percent of 455 VHA facilities reported they met both requirements, with the remainder meeting one or none of the requirements. VHA officials said that regional networks are responsible for monitoring their facilities' adherence to the requirements and developing corrective action plans. However, VHA does not monitor implementation of corrective action plans. Doing so would ensure facilities are taking appropriate actions to comply. Veterans at those facilities would then have better access to mental health care services in primary care settings, as VHA intends.
VHA facilities reported that persistent staffing challenges have adversely affected their efforts to integrate mental health services into primary care settings from 2016 through February 2022 (see figure).
Percentage of VHA Facilities That Reported Staffing As Their Most Significant Challenge, 2016 through 2022
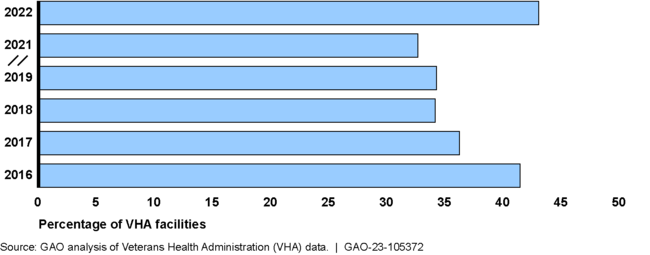
Note: Data were reported in VHA annual surveys. According to VHA officials they did not administer a 2020 annual survey due to the COVID-19 pandemic.
To address staffing challenges, officials from the selected facilities in GAO's review reported taking steps such as offering more flexible work schedules and providing additional technology to reduce workloads. Regional network officials identified several additional strategies that VHA could consider, such as providing additional guidance on recruiting and retaining staff and increasing funding for certain positions. Evaluating and implementing these strategies, and any others as appropriate, may help facilities mitigate staffing challenges. Doing so would help ensure that veterans receive the most appropriate and timely mental health care services available.
Why GAO Did This Study
VHA has seen a significant increase in demand for mental health services and expects that demand to continue to grow. One way VHA meets such demand is by integrating certain mental health services within primary care settings.
The Commander John Scott Hannon Veterans Mental Health Care Improvement Act of 2019 included a provision for GAO to review VHA's integration of primary and mental health services. Among other objectives, this report examines the extent to which facilities have met VHA requirements to integrate mental health care into primary care. It also discusses challenges that have affected such integration and steps VHA has taken to mitigate them.
GAO reviewed VHA documentation and policies on integration efforts and annual survey data from 2011 to 2022. GAO also interviewed VHA officials and providers from nine VHA facilities. These facilities were selected based on geographic location and other factors, such as the percentage of veterans receiving integrated mental health services in fiscal year 2020.
Recommendations
GAO is recommending that VHA (1) monitor the development and implementation of corrective action plans and (2) evaluate and implement strategies to help mitigate staffing challenges affecting the integration of mental health and primary care services. VA concurred with GAO's recommendations and described steps it has or plans to take to implement them.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Veterans Health Administration | The Under Secretary for Health should ensure that the Office of Mental Health and Suicide Prevention monitors VISNs' development and implementation of corrective action plans for any VHA facilities that do not fully adhere to VHA's Primary Care Mental Health Integration program requirements. (Recommendation 1) |
VA concurred with this recommendation . In October 2024, VA stated that the Office of Mental Health (OMH - formerly the Office of Mental Health and Suicide Prevention) has begun monitoring Veterans Integrated Service Networks' (VISN) development and implementation of corrective action plans for any VHA facilities that do not fully adhere to VHA's Primary Care Mental Health Integration program requirements. In March 2024, VHA issued a directive establishing VHA program offices' responsibilities for issuing, monitoring, and evaluating waivers to national policies, including its Primary Care Mental Health Integration program . Through this directive, OMH allows VISNs to submit temporary waiver requests and keep OMH advised of continued noncompliance or progress made toward completing action plans. VA stated that OMH will use a standardized dashboard to track waivers and will also review the status of waiver requests on a quarterly basis. VA reported that VISNs and/or VHA facilities demonstrating noncompliance, or a lack of progress, may face further action from higher levels of management, such as VHA's Audit, Risk and Compliance Committee or its Governing Board for assistance with mitigation and resolution if needed. As a result of these actions, we are closing this recommendation as implemented.
|
| Veterans Health Administration | The Under Secretary for Health should ensure that the Office of Mental Health and Suicide Prevention comprehensively evaluate and implement strategies to help mitigate staffing challenges that affect VHA facilities' abilities to integrate mental health care within primary care settings. (Recommendation 2) |
VA concurred with this recommendation. In May 2023, VA stated that it had evaluated its current strategies to help mitigate staffing challenges that affect VHA facilities' abilities to integrate mental health care within primary care settings and established an action plan to consider further implementation of those strategies. In June 2024, VHA released a memorandum outlining its Mental Health Optimization and Outpatient Staffing Enhancement Initiative. This initiative provides guidance to Veterans Integrated Services Network (VISN) directors to support VHA facilities and VISNs as they develop strategic plans to optimize mental health staffing across the continuum of care, including primary care mental health integration. The initiative provides resources for each facility and VISN to designate a workgroup to address existing mental health staffing requirements and establish a strategic staffing plan sufficient to meet upcoming projected demand for mental health services. Specifically, each facilities' staffing plan is to include an estimate of staff needed over the next five years and specific strategies for recruiting and retaining mental health staff. VHA stated it plans to use information from the staffing plans to inform future budget decisions and develop updated projections and planning tools annually over five years. As a result of these actions, we are closing this recommendation as implemented.
|
