VA Health Care: Veterans' Use of Long-Term Care Is Increasing, and VA Faces Challenges in Meeting the Demand
Fast Facts
Veterans rely on long-term care from the VA for everything from occasional help around the house to round-the-clock care. Eligibility is primarily based on the extent of a service-connected disability.
Demand for long-term care increased 14% and VA’s expected spending went up 33% from FY 2014-2018. VA projects demand will continue to increase and spending will double by 2037.
VA faces 3 key challenges to meeting long-term care needs: finding enough workers, providing care where geographically needed, and providing specialty care.
We made 3 recommendations, including that VA develop measurable goals in these areas.
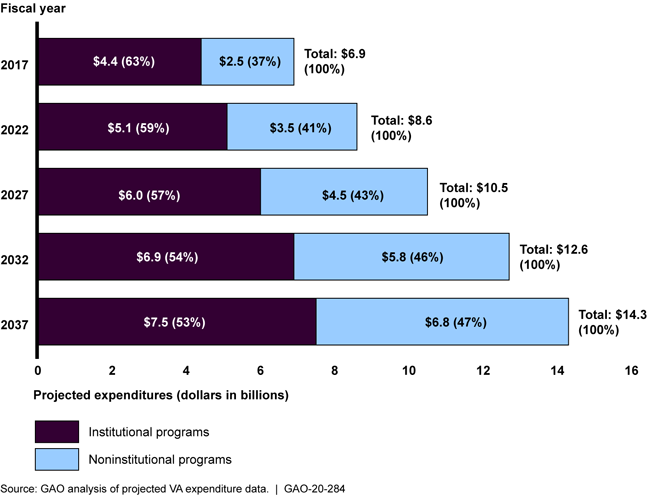
Projected Expenditures for Department of Veterans Affairs’ Long-Term Care Programs, Fiscal Years 2017 through 2037
Bar chart
Highlights
What GAO Found
The Department of Veterans Affairs (VA) provides or purchases long-term care for eligible veterans through 14 long-term care programs in institutional settings like nursing homes and noninstitutional settings like veterans' homes. From fiscal years 2014 through 2018, VA data show that the number of veterans receiving long-term care in these programs increased 14 percent (from 464,071 to 530,327 veterans), and obligations for the programs increased 33 percent (from $6.8 to $9.1 billion). VA projects demand for long-term care will continue to increase, driven in part by growing numbers of aging veterans and veterans with service-connected disabilities. Expenditures for long-term care are projected to double by 2037, as shown below. According to VA officials, VA plans to expand veterans' access to noninstitutional programs, when appropriate, to prevent or delay nursing home care and to reduce costs.
VA Projections for Long-Term Care Expenditures, Fiscal Years 2017 through 2037
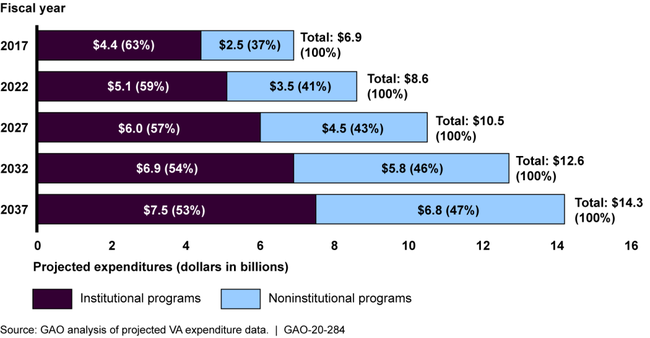
Note: These long-term care programs include those VA projects using its Enrollee Health Care Projection Model. This model includes 12 of VA’s 14 Long-Term Services and Supports programs, excluding State Veterans Homes and State Home Adult Day Health Care.
VA currently faces three key challenges meeting the growing demand for long-term care: workforce shortages, geographic alignment of care (particularly for veterans in rural areas), and difficulty meeting veterans' needs for specialty care. VA's Geriatrics and Extended Care office (GEC) recognizes these challenges and has developed some plans to address them. However, GEC has not established measurable goals for these efforts, such as specific staffing targets for programs with waitlists or specific targets for providing telehealth to veterans in rural areas. Without measurable goals, VA is limited in its ability to address the challenges it faces meeting veterans' long-term care needs.
Why GAO Did This Study
Veterans rely on long-term care to address a broad spectrum of needs, from providing occasional help around the house to daily assistance with eating or bathing to round-the-clock clinical care. Veterans' eligibility for this care is primarily based on their service-connected disability status, among other factors. Congress included a provision in statute for GAO to review VA's long-term care programs. This report (1) describes the use of and spending for VA long-term care and (2) discusses the challenges VA faces in meeting veterans' demand for long-term care and examines VA's plans to address those challenges. GAO reviewed VA documents, such as strategic planning documents for long-term care programs and analyzed VA utilization and expenditure data for fiscal years 2014 through 2018 (the latest available at the time of the review) and projected data through 2037. GAO also interviewed officials from VA, including officials from VA's GEC, which is responsible for overseeing long-term care programs; and from Veterans Service Organizations.
Recommendations
GAO is making three recommendations, including that VA develop measurable goals for its efforts to address key challenges in meeting the demand for long-term care. VA concurred with GAO's recommendations and identified actions it will take to implement them.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Office of the Secretary for VA | The Secretary of VA should direct GEC leadership to develop measurable goals for its efforts to address key long-term care challenges: workforce shortages, geographic alignment of care, and difficulty meeting veterans' needs for specialty care. (Recommendation 1) |
VA concurred and in December 2021 provided information describing actions it has taken to develop measurable goals for efforts that can help address the key long-term care challenges identified in our work. Specifically, GEC, in collaboration with other VHA offices, outlined some measurable goals for workforce shortages, geographic alignment of care, and difficulty meeting veterans' needs for specialty care. For each goal, GEC set time frames for completion with targeted completion dates ranging from 2021 to 2026. While we have closed this recommendation as implemented, these are complex and persistent long-term care challenges for VA (and others) and we encourage VA to remain vigilant in its efforts.
|
| Office of the Secretary for VA | The Secretary of VA should direct GEC leadership to set time frames for and implement a consistent GEC structure at the VAMC level. (Recommendation 2) |
VA concurred, and in 2022 described and provided documents about the alignment of GEC programs at the VISN level through its Rehabilitation and Extended Care Integrated Clinical Community structure. In 2023, VA described and provided documents about the alignment of GEC programs at the VAMC level through primary care teams. Specifically, VA's GEC officials described how veterans seeking care through GEC programs will primarily access this care through consultations with their primary care teams. The primary care teams will discuss GEC options-including institutional and non-institutional programs-and prepare a standardized consultative assessment on what care the veteran wants. This consultative assessment is then sent to the VAMC's GEC coordinator for processing. In instances where a discussion of care options initially occurs outside of primary care-for example in inpatient discharge planning with a social worker-social workers will refer the veteran to a primary care provider to prepare the GEC consultative assessment. Officials noted that by having primary care providers, who have access to training on VA's long-term care programs, as the hub of veteran long-term care provision, veterans will have a more consistent experience accessing long-term care through VAMCs.
|
| Office of the Secretary for VA | The Secretary of VA should direct GEC leadership to set time frames for and implement a VAMC-wide standardization of the tool for assessing the noninstitutional program needs of veterans. (Recommendation 3) |
VA concurred and in a January 2022 update indicated that the case mix tool was available for use by all staff and that trainings were held in November 2021. In a March 2022 memo, VA noted that effective May 1, 2022 all VAMCs were required to exclusively use the case mix tool when making personal care services referrals.
|
