VA Disability Compensation: Actions Needed to Enhance Information about Veterans' Health Outcomes
Fast Facts
The Department of Veterans Affairs pays monthly compensation to veterans with disabling conditions caused or aggravated by their military service.
We found that more than half of the veterans receiving disability compensation used VA health care for their conditions. However, VA does not have a clear picture of whether these services improve veterans’ health. VA could also enhance its process for determining when to reevaluate possible changes in health conditions.
We made 5 recommendations, including that VA develop better research on health outcomes for veterans receiving disability pay and improve its reevaluation process.

Military ID tags and US flag
Highlights
What GAO Found
In fiscal year 2018, about 54 percent of veterans receiving Department of Veterans Affairs (VA) disability compensation had at least one VA outpatient visit to treat an injury or illness that VA deemed was incurred or aggravated during military service (i.e., a service-connected condition). However, the health outcomes of veterans with service-connected conditions, such as changes in the severity of symptoms or the incidence of mortality, are not well understood. Information about health outcomes is central to ensuring veterans' wellness and assessing improvement in their disability status. According to VA researchers GAO spoke with and academic studies GAO reviewed, various challenges have limited research on this population. For example, data reside in different VA systems and use different identifiers for medical conditions, hindering use of the data. While VA has begun to consider ways to analyze health outcomes, it has not yet established a plan for this effort, including the scope, specific activities, and timeframes for addressing the identified research challenges.
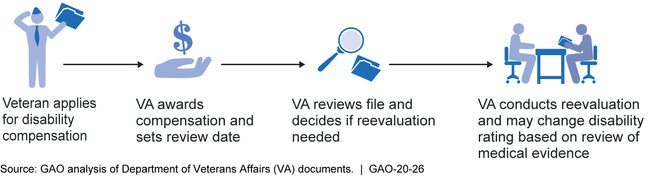
VA does not glean information from the results of reevaluations to help manage its disability compensation program. Disability reevaluations help VA gauge whether veterans' service-connected conditions have changed, and whether disability compensation should be modified to reflect those changes (see figure).
VA Disability Compensation Reevaluation Process
However, VA does not fully use key management information, such as:
- trends in how frequently certain conditions are reevaluated, including those required by VA regulations to be reevaluated; and
- outcomes of reevaluation decisions for individual conditions (i.e., whether conditions worsened or improved).
Both trend and outcome information could help VA better target its resources toward reevaluating conditions more likely to change.
VA recently updated its procedures manual to specify which staff may determine whether a veteran's condition should be reevaluated, but has not clearly defined skill sets and training needed to consistently implement these procedures. Specifically, the updated procedures do not indicate the knowledge, skills, and abilities staff need to determine when to conduct reevaluations. Further, VA has not ensured that training aligns with these needed skillsets. Without improving procedures and training, VA is at risk of conducting unnecessary reevaluations and burdening veterans.
Why GAO Did This Study
VA receives billions of dollars per year to provide health care and disability compensation to promote the wellness of veterans with service-connected conditions. VA studies veterans' health through research and assesses changes in service-connected conditions through its reevaluation process.
GAO was asked to review VA's efforts to study and gauge the health outcomes of veterans with service-connected conditions. This report examines the extent to which (1) veterans used VA health care services to treat service-connected conditions, and what is known about their health outcomes; (2) VA uses information on reevaluations to help manage the program; and (3) VA's procedures position it to determine when to conduct a reevaluation.
GAO reviewed fiscal year 2018 VA health care data; selected studies; VA data on completed reevaluations from fiscal years 2013-2018; and relevant federal laws, regulations, and program guidance. GAO also interviewed staff at four VA regional offices (selected for variation in claims workload and location) and VA officials at the agency's central office.
Recommendations
GAO is making five recommendations, including that VA develop a plan to address challenges to studying health outcomes, use information on reevaluations to improve program management, and improve procedures and training for reevaluations. VA agreed with two recommendations and agreed in principle with the other three, but its proposed actions do not fully address GAO's concerns.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Department of Veterans Affairs | The Secretary of Veterans Affairs should ensure that the Office of Enterprise Integration develops a plan—including milestones and roles and responsibilities for OEI, VBA, and VHA—to address identified challenges that have hindered research on the health care outcomes for service-connected conditions of veterans receiving disability compensation. To align VA's efforts with the goals of its 2018-2024 Strategic Plan, VA's development of this plan should be completed and ready for implementation by June 1, 2020. (Recommendation 1) |
VA agreed with this recommendation. In 2024, VA revised its plan to address the challenges hindering research. This plan includes milestones, roles and responsibilities that address challenges we described in our report. For example, one key challenge is that VBA and VHA data do not use the same identifiers for medical conditions that are needed to link the two information sources. VA's plan describes a completed milestone to develop an approach to link the two information sources, starting with an initial set of certain conditions associated with the PACT Act. These conditions include cancer and chronic respiratory diseases associated with toxic exposure. Also, VA's Learning Agenda describes a current project using a dataset of VBA disability claims information and data on VA and non-VA health care, in order to obtain a more complete picture of health care utilization by veterans with service-connected conditions. This effort is referenced in VA's Strategic Plan, which states this effort to assess trends in PACT Act-eligible veterans' health care utilization will be completed by September 30, 2025. VA's efforts to address research challenges could help improve the agency's ability to better understand health outcomes for veterans receiving disability compensation.
|
| Department of Veterans Affairs | The Under Secretary for Benefits should develop and implement a periodic analysis of program management data for trends in the individual service-connected conditions being reevaluated as well as data on the outcomes of reevaluations. (Recommendation 2) |
VA concurred with this recommendation. In December 2021, VA officials stated that they analyzed trends in reevaluation of individual service-connected conditions and on the outcomes of reevaluations for fiscal years 2018 through 2020. Based on the findings from its analyses, in October 2021, VA released a Policy Letter stating that reevaluations should only be conducted when required by its disability rating criteria (i.e., the VA Schedule for Rating Disabilities) for specific conditions, or when necessary to reduce a rating. VBA officials estimate that this policy change will result in approximately 80,000 reevaluations not being initiated each year. Also in October 2021, VBA cancelled reevaluations in which disability rating criteria did not require them, which resulted in a 70 percent reduction in pending reevaluations. In February 2022, officials reported that unnecessary pending reevaluations are cancelled on a monthly basis based on specific diagnostic code criteria, and that the analysis and oversight of the pending reevaluations will continue on a monthly basis.
|
| Department of Veterans Affairs | The Under Secretary for Benefits should implement the two recommendations in VBA's May 2018 consistency study to provide training on how to determine when a reevaluation is needed and review reevaluation decisions for accuracy at the lowest-scoring offices and take corrective action as needed. (Recommendation 3) |
VA concurred with this recommendation. VA's updated action plan states the agency will conduct periodic reviews of reevaluations to ensure accuracy, and document the findings and the need for corrective action, if any. VA stated it has conducted a review of the lowest-scoring offices identified in the 2018 study, and found these offices' accuracy rates for reevaluations were all above 94 percent. Prior to this review, in fall 2019, VA provided training to claims processors on reevaluations. In 2021, the agency issued updated guidance detailing the limited instances when a reevaluation should be conducted, and reviewed its pending reevaluations to cancel those that were not warranted.
|
| Department of Veterans Affairs | The Under Secretary for Benefits should clarify guidance in its procedures manual regarding the knowledge, skills, and abilities needed to make decisions on whether to reevaluate veterans for changes in their service-connected conditions. (Recommendation 4) |
VA agreed with this recommendation in principle, acknowledging the importance of having appropriately skilled and trained employees to process reevaluations and other claims. To address the recommendation, VA took several actions. Specifically, VA conducted a targeted accuracy review of routine future examinations by non-raters, which showed an 85 percent accuracy rate. Based on this review, VA simplified reevaluation requirements and clarified its guidance through publication of Policy Letter 21-01. In addition, VA updated its training for raters with the knowledge needed to properly process reevaluations in September 2021. More recently, VA issued a reminder to all claims processors who process reevaluations about the required training and updated guidance. Regional offices also continued to identify and validate employee expertise through individual quality reviews. These reviews allow the regional office to assess employee proficiency and error trends, and assign training as needed. These actions to simplify the reevaluation guidelines, update the training, and conduct monthly quality reviews position VA to ensure that claims processors have the knowledge, skills, and abilities to conduct reevaluations according to VBA guidance.
|
| Department of Veterans Affairs | The Under Secretary for Benefits should align training requirements with the knowledge, skills, and abilities needed for reviewing claims to decide whether to conduct a reevaluation. (Recommendation 5) |
VA agreed with this recommendation in principle. In February 2021, VA officials told us that VBA planned to conduct a targeted accuracy review of routine future examinations requested by claims processors and would review the results to determine if any additional training for claims processors was needed. This accuracy review, conducted in October and November 2020, showed an 85 percent accuracy rate for non-raters. Based on results of this accuracy review, VA officials told us that Compensation Service provided training to all claims processors in March and April to improve their knowledge and skill in processing reevaluations. Specifically, the training reviewed the errors identified in the targeted accuracy review and VA's policies for determining whether a reevaluation is needed. VA also identified scenarios when reevaluations were requested, but were not warranted to help guide claims processors' ability to make reevaluation decisions.
|
