VA Mental Health: VHA Improved Certain Prescribing Practices, but Needs to Strengthen Treatment Plan Oversight
Fast Facts
VA's mental health care providers have options, such as medication and therapy, to treat veterans with mental health conditions. VA has taken steps to improve mental health treatment, such as prescribing medications with dangerous side effects less frequently.
However, VA doesn't monitor whether providers are documenting that they have considered different options before deciding on a treatment plan, as guidance suggests.
Providers are also supposed to document treatment plans in an easily identifiable way in veterans' medical records, but VA hasn't given them guidance on how to do this.
We recommended that VA address these issues.
Treatments for Mental Health Conditions by Type
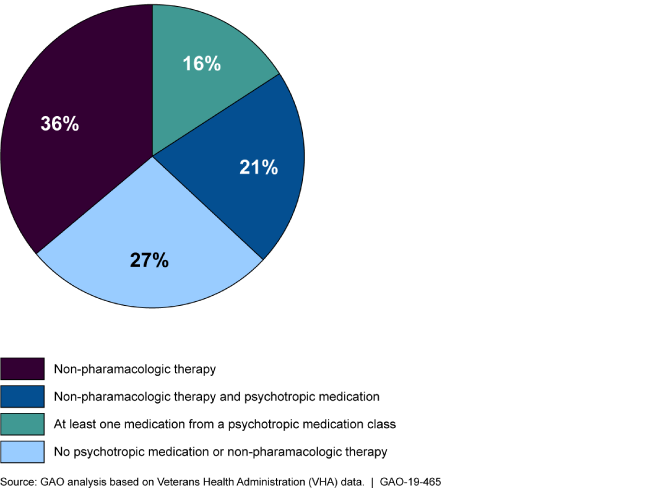
Pie chart showing the percentage of veterans receiving each type of treatment.
Highlights
What GAO Found
Officials from the five selected Department of Veterans Affairs (VA) medical centers (VAMC) GAO spoke with reported various factors that contribute to providers' mental health treatment decisions, including decisions regarding the prescribing of psychotropic medications and the offering of non-pharmacologic therapy. Examples of reported factors include: VAMC resources, such as the availability of appointments with mental health providers in specialty care, and the complexity of veterans' mental health conditions, such as the veterans' diagnoses and treatment history.
Officials with VA's Veterans Health Administration (VHA) told GAO that specialty mental health care providers are expected to document mental health treatment plans in an easily identifiable way in veterans' medical records, but VHA has not developed guidance explicitly addressing this expectation. For example, VHA's mental health services handbook requires that treatment plans include certain components, but does not specify where to document the plan within a veteran's medical record. As a result, there is a risk that a provider may be unable to readily access information about a veteran's mental health treatment, including the use of medication or therapy, during changes in a veteran's care.
VHA has not monitored whether mental health providers in specialty care document the required consideration of different treatment options—such as psychotropic medications or non-pharmacologic therapy—within mental health treatment plans. VHA officials told GAO that VHA relies on the Joint Commission (an independent, not-for-profit organization that accredits and certifies health care organizations) to assess specialty mental health treatment plans as part of the organization's accreditation process for each VAMC. However, the Joint Commission's standards do not specifically assess whether providers consider different treatment options. As a result, VHA cannot ensure that providers are considering all available treatment options and providing the most appropriate treatments to each veteran.
VHA has taken steps to improve veterans' mental health treatment through the Psychotropic Drug Safety Initiative (PDSI)—an initiative focused on the safe and effective prescribing of certain psychotropic medications. For example, the first phase included a performance metric aimed at decreasing the percentage of veterans with post-traumatic stress disorder receiving one or more outpatient prescriptions for a benzodiazepine (a medication used to treat anxiety) because of risks associated with the medication. VHA reported a nationwide 5.4 percentage point decrease in the prescribing of this medication for these patients, as well as improvements in the majority of the initiative's other performance metrics.
Why GAO Did This Study
In fiscal year 2018, of the roughly 6 million veterans who received services from VHA, approximately 2 million had a diagnosis for at least one mental health condition. Treatments for such mental health conditions can include psychotropic medications or non-pharmacologic therapies, which can be prescribed or offered by VA providers in outpatient settings including primary and specialty care.
GAO was asked to review how mental health treatment decisions are made by providers in VAMCs and monitored by VHA. This report examines, among other things, (1) factors that contribute to providers' treatment decisions for veterans with mental health conditions, (2) VHA's guidance for documenting mental health treatment plans, (3) VHA's monitoring of whether providers document their consideration of different treatment options, and (4) VHA's efforts to improve the treatment of veterans prescribed psychotropic medications. GAO reviewed VHA documents and a nongeneralizable sample of veterans' medical records from five VAMCs (selected for variety in facility complexity and location); analyzed data on psychotropic medication prescribing; and interviewed VHA and VAMC officials.
Recommendations
VHA should (1) disseminate guidance reflecting its expectation that providers document mental health treatment plans in an easily identifiable way, and (2) implement an approach for monitoring whether these treatment plans include consideration of treatment options. VHA agreed with GAO's recommendations.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Veterans Health Administration | The Veterans Health Administration should disseminate guidance for VISNs and VAMCs that more clearly reflects its expectation that mental health providers in specialty care should record mental health treatment plans within veterans' medical records in an easily identifiable way. (Recommendation 1) |
VHA concurred with this recommendation and provided updates on its progress in implementing it. In October 2020, VHA provided us with a memorandum dated May 2019 regarding mental health treatment planning that explicitly states the requirement for mental health providers in specialty care to record mental health treatment plans as a separate, easily identifiable document in the medical record. According to this memorandum, these treatment plans are expected to ensure that it is clear what treatment is being provided, that different treatments were considered, and that ongoing assessments are used to determined whether treatment changes are needed for the patient. The memorandum also states that facilities must either use the current treatment planning software or another method to create such a plan. Finally, the memorandum requires VAMCs to attest to full implementation of these requirements within 45 days of receipt of the memorandum. VHA provided us with evidence of attestation from all VISNs, on behalf of the VAMCs within their networks, indicating full implementation of the process. As such, we are closing this recommendation as implemented.
|
| Veterans Health Administration |
Priority Rec.
The Veterans Health Administration should develop and implement an approach for monitoring treatment plans for veterans with mental health conditions to ensure that such plans include documentation that different evidence-based treatment options were considered. (Recommendation 2) |
VHA concurred with this recommendation and provided updates on its progress in implementing it. In October 2020, VHA provided us with a memorandum regarding mental health treatment planning that explicitly states the requirement for mental health providers in specialty care to record mental health treatment plans that include (among other things) an indication that different treatments were considered. The memorandum also requires VAMCs to implement ongoing chart reviews to ensure providers are meeting treatment planning expectations. The memorandum requires all VAMCs to ensure that each licensed independent provider has 5 treatment plans reviewed biannually to determine whether treatment planning expectations were achieved, including whether different evidence-based treatments were considered. Finally, the memorandum requires VAMCs to attest to full implementation of this process within 45 days of receipt of the memorandum. VHA provided us with evidence of attestation from all VISNs, on behalf of the VAMCs in their networks, indicating full implementation of the process. VHA told us the results of the biannual reviews are used locally for performance plans and compliance with accreditation standards. As such, we are closing this recommendation as implemented.
|
