Veterans Choice Program: Further Improvements Needed to Help Ensure Timely Payments to Community Providers
Fast Facts
The VA's Veterans Choice Program allows veterans to get health care from providers not directly employed by VA (community providers), such as when facing long wait times at VA facilities.
VA uses contractors to pay providers for their services to veterans. But contractor payment times have varied, sometimes causing delays in providers' payments. The result: providers may not want to continue participating in the Choice Program, which may decrease veterans' access to health care.
A Veterans Community Care Program to replace the Choice Program is to begin in 2019. We recommended that VA take steps to correct provider payment issues.
A photo of a patient getting their blood pressure checked.
Highlights
What GAO Found
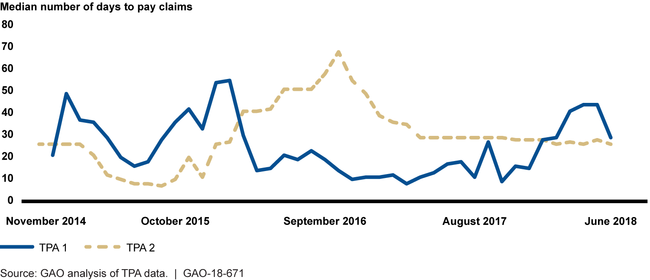
The Department of Veterans Affairs' (VA) Veterans Choice Program (Choice Program) was created in 2014 to address problems with veterans' timely access to care at VA medical facilities. The Choice Program allows eligible veterans to obtain health care services from providers not directly employed by VA (community providers), who are then reimbursed for their services through one of the program's two third-party administrators (TPA). GAO's analysis of TPA data available for November 2014 through June 2018 shows that the length of time the TPAs took to pay community providers' clean claims each month varied widely—from 7 days to 68 days. VA and its TPAs identified several key factors affecting timeliness of payments to community providers under the Choice Program, including VA's untimely payments to TPAs, which in turn extended the length of time TPAs took to pay community providers' claims; and inadequate provider education on filing claims.
Median Number of Days to Pay Clean Claims through VA's Third Party Administrators (TPA), November 2014 through June 2018
VA has taken actions to address key factors that have contributed to the length of time TPAs have taken to pay community providers. For example, VA updated its payment system and related processes to pay TPAs more quickly. According to VA data, as of July 2018, VA was paying at least 90 percent of the TPAs' invoices within 7 days. In addition, VA and the TPAs have taken steps to improve provider education to help providers resolve claims processing issues. However, 9 of the 15 providers GAO interviewed said they continue to experience lengthy telephone hold times. According to VA and TPA officials, steps have been taken to improve the customer service offered to community providers. However, VA officials do not collect data on or monitor TPA compliance with customer service requirements—such as calls being answered within 30 seconds or less—for provider calls because they said they are not enforcing the requirements and are allowing TPAs to prioritize calls from veterans. Without collecting data and monitoring compliance, VA does not have information on challenges providers may face when contacting TPAs to resolve payment issues.
Why GAO Did This Study
Questions have been raised about the lack of timeliness of TPAs' payments to community providers under the Choice Program and how this may affect the willingness of providers to participate in the program as well as in the forthcoming Veterans Community Care Program. You asked GAO to review issues related to the timeliness of TPAs' payments to community providers under the Choice Program.
This report examines, among other things, (1) the length of time TPAs have taken to pay community providers' claims and factors affecting timeliness of payments, and (2) actions taken by VA and the TPAs to reduce the length of time TPAs take to pay community providers for Choice Program claims.
GAO reviewed TPA data on the length of time taken to pay community provider claims from November 2014 through June 2018, the most recent data available at the time of GAO's review. GAO also reviewed documentation, such as the contracts between VA and its TPAs, and interviewed VA and TPA officials. In addition, GAO interviewed a non-generalizable sample of 15 community providers, selected based on their large Choice Program claims volume, to learn about their experiences with payment timeliness.
Recommendations
GAO is making two recommendations, including that VA should collect data on and monitor compliance with its requirements pertaining to customer service for community providers. VA concurred with GAO's recommendations and described steps it will take to implement them.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Department of Veterans Affairs | Once VA's new software for managing authorizations has been fully implemented, the Undersecretary for Health should monitor data on secondary authorization requests approval decision time frames to ensure VA medical facilities are in adherence with VA policy, assess the reasons for nonadherence with the policy, and take corrective actions as necessary. (Recommendation 1) |
VA agreed with our recommendation. In February 2023, VA officials stated that they created a secondary authorization request/request for services report in their Consult Toolbox to monitor data on approval decision time frames. The report documents the average number of days from the date requests are received to the date the approval decision/outcome is entered. The report is available for use in by field staff, and is reviewed during VA central office site visits to VA medical centers. When VA medical centers are not adhering to policy, a corrective action plan is developed and monitored by VA central office through to completion. VA provided examples of the request for services report, and a corrective action in place at one VA medical center. Based on VHA's actions, we are closing this recommendation.
|
| Department of Veterans Affairs | The Undersecretary for Health should collect data and monitor compliance with the Choice Program contractual requirements pertaining to customer service for community providers, and take corrective actions as necessary. (Recommendation 2) |
VA agreed with our recommendation and stated that, at the time, it did not have the ability to monitor and assess the performance of customer service operations under the Choice Program contracts. Instead, VA included customer service metrics in its Community Care Network (CCN) contracts for the Veterans Community Care Program, and plans to monitor compliance with these requirements. VA has awarded contracts for 5 of the 6 CCN Regions (which include customer service metrics), and plans for the last contract to include the same metrics to be consistent throughout the CCN. Until the contract for Region 6 is awarded, VA stated that the interim contract contains customer service metrics in order to deliver customer support. In addition, VA's CCN contracts include a process for VA to monitor the contractors' customer service metrics and issue corrective action plans, when needed. If issued a corrective action plan, the contractor must report corrective actions and associated improvements to VA on a monthly and quarterly basis, including its plan and timeframe for resolving the issue. Based on VA's actions, we are closing this recommendation.
|
