Urban Hospitals: Factors Contributing to Selected Hospital Closures and Related Changes in Available Health Care Services
Fast Facts
About half of U.S. hospitals are in urban areas. More urban hospitals closed than opened from 2019 to 2023.
All of the 5 hospitals in our review struggled financially before they closed, with inpatient volumes decreasing at 4 of them. The anticipated cost of upgrading or maintaining aging facilities also contributed to the closures of all 5 hospitals.
After closure, 2 of the hospitals still provided outpatient services, while the other 3 stopped all services.
Representatives from local hospitals, providers, and community organizations told us some community residents continued having trouble getting health care after all 5 hospitals closed.
An Empty Patient Room Used as Storage

Highlights
What GAO Found
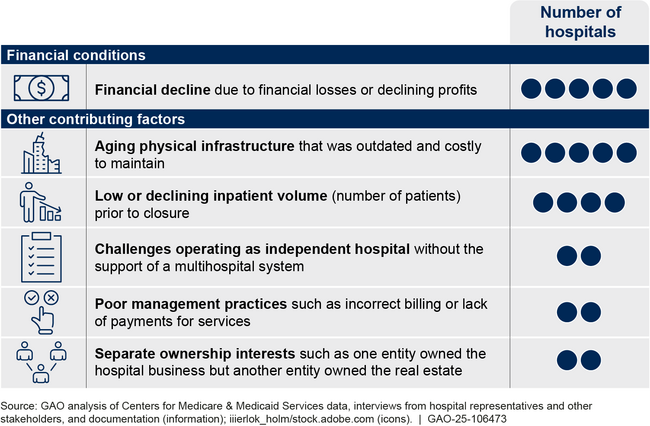
All five urban hospitals included in GAO's review experienced financial decline characterized by financial losses or declining profits in the 5 years leading to their closure. For instance, one hospital filed for bankruptcy under three different owners within 5 years prior to its closure. Several other factors contributed to hospital financial decline and closure such as aging physical infrastructure, low inpatient volume, challenges operating as independent hospitals, poor management practices, and separate ownership interests.
Factors Contributing to Closure of Five Selected Urban Hospitals in 2022 or 2023
The availability of health care services shifted or decreased in the communities of all five hospitals after the hospitals closed. Specifically, two hospitals continued providing outpatient services after closing their inpatient services, and other providers in their communities adjusted their service availability by, for example, expanding inpatient capacity, according to stakeholders. The other three hospitals ceased all health care services when they closed. After two of them closed, the decline in service availability affected nearby hospitals and community residents. For example, one hospital's closure reduced the availability of emergency and inpatient services in the part of the city where it was located, which exacerbated pre-existing access to care challenges for community residents, according to stakeholders.
Stakeholders for all five hospitals identified ongoing challenges with access to health care that some residents in their communities continued to experience after the closures. For example, even though the community residents had several options to seek health care after the hospitals closed, some residents lacked adequate transportation to reach alternative facilities or lacked access to primary care providers, according to stakeholders.
Why GAO Did This Study
Hospitals play a critical role in delivering health care services to their communities. Approximately half of U.S. hospitals are in urban areas, and closures of urban hospitals outpaced new openings from 2019 to 2023. GAO and others have previously reported on hospital closures in rural areas, but few studies have been conducted on the closure of urban hospitals.
GAO was asked to examine the bankruptcy and closure of health care facilities. This report describes the closure of five selected urban hospitals, specifically: (1) the financial conditions and other factors that contributed to their closure and (2) how health care service availability in communities changed after their closure. GAO selected a nongeneralizable sample of five hospitals in urban areas that closed in 2022 or 2023. These five selected urban hospitals reflect variation in geographic region, ownership type (for-profit vs. nonprofit), and whether the hospital provided outpatient services after it closed. GAO analyzed financial data on each hospital from the Department of Health and Human Services and reviewed relevant documents including information provided by selected hospitals and publicly available information such as court documents or community health needs assessments. GAO interviewed representatives from these selected hospitals and other stakeholders, such as representatives from nearby hospitals, other health care providers, community organizations, state hospital associations, and local government officials. In addition, GAO visited two selected hospitals.
For more information, contact Leslie V. Gordon at GordonLV@gao.gov.
