Medicare Cognitive Assessments: Utilization Tripled between 2018 and 2022, but Challenges Remain
Fast Facts
More than 10 million Americans age 65 and older live with a cognitive impairment, such as Alzheimer's disease.
Medicare offers a service in which health care providers diagnose cognitive impairments and develop a plan to manage them. Use of the service tripled from 2018-2022. But we calculated that in 2021, a maximum 2.4% of traditional Medicare beneficiaries with an Alzheimer's disease diagnosis may have received the service.
Usage may be low because:
Many providers schedule in 15-20 minute blocks so finding an hour or more needed for the service is difficult
Beneficiaries may not know about it
There is stigma associated with diagnosis

Highlights
What GAO Found
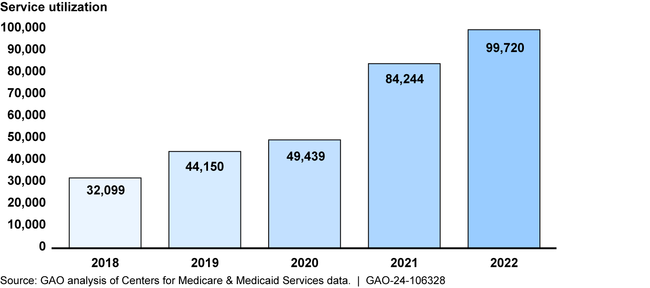
“Cognitive assessment and care plan services” is a service available to Medicare beneficiaries in which providers diagnose and develop a plan to manage cognitive impairments, such as Alzheimer's disease. Providers typically need 60 minutes of face-to-face time to deliver the cognitive assessment service, which includes a cognitive assessment and care plan. GAO found that use of the service in traditional fee-for-service Medicare tripled from 2018 through 2022. However, a relatively small number of Medicare beneficiaries diagnosed with a cognitive impairment received the service. GAO calculated that, at most, in 2021, about 2.4 percent of traditional Medicare beneficiaries with a diagnosis of Alzheimer's disease or a related disorder may have received the service. Similar services can be delivered during other types of visits, such as through evaluation and management visits. GAO found that from 2018 through 2022, certain types of providers—neurologists, nurse practitioners, internists, family physicians, and geriatricians—delivered more than 80 percent of services, mostly in urban locations.
Annual Utilization of the Cognitive Assessment Service in Traditional Medicare, 2018 through 2022
Stakeholders described various challenges faced by providers delivering the cognitive assessment service and beneficiaries trying to access the service. Provider challenges include (1) the time needed, particularly for providers who typically schedule 15-20-minute visits; (2) billing limitations that prevent providers working in teams to collaborate on the service visit; and (3) limited training for primary care providers. Beneficiary advocacy groups described access challenges including the stigma associated with being diagnosed with a cognitive impairment and lack of awareness of the service.
To increase awareness of the cognitive assessment service, the Centers for Medicare & Medicaid Services (CMS), the agency within the Department of Health and Human Services (HHS) that administers the Medicare program, conducted a provider outreach campaign targeting 1.4 million providers eligible to deliver the service. Additionally, to increase awareness among beneficiaries, the agency added a description of the service to the Medicare.gov website and the Medicare & You handbook.
Why GAO Did This Study
The number of Medicare beneficiaries living with a cognitive impairment, such as Alzheimer's disease, is projected to increase as the American population age 65 and older grows. Such beneficiaries' health care costs are also projected to increase.
CMS began covering the cognitive assessment and care plan services visit in 2017 to increase access to cognitive care services in Medicare.
The Consolidated Appropriations Act, 2021, includes a provision for GAO to review use of the cognitive assessment service in the Medicare program. This report describes (1) utilization of the cognitive assessment service in traditional Medicare from 2018 through 2022; (2) stakeholder views on challenges providers face delivering and beneficiaries face accessing the service; and (3) steps CMS has taken to increase awareness of the service.
GAO analyzed claims and enrollment data from traditional fee-for-service Medicare from 2018 through 2022 to identify service utilization.
GAO interviewed officials representing seven stakeholder groups regarding access and delivery challenges. Organizations included the American Academy of Family Physicians and AARP. GAO also scanned literature to identify research on access challenges; and interviewed agency officials regarding the agency's outreach campaign. GAO provided a draft of this report to HHS.
For more information, contact Leslie V. Gordon at (202) 512-7114 or GordonLV@gao.gov.
