Health Insurance Exchanges: HHS Should Enhance Its Management of Open Enrollment Performance
Fast Facts
We examined 2018 enrollment in Affordable Care Act health insurance exchanges and federal efforts to encourage enrollment.
We found:
About 8.7 million people bought insurance in 2018 through the federal website (healthcare.gov), 5% less than in 2017.
Health and Human Services reduced its advertising and other consumer outreach. The 23 stakeholders we interviewed had mixed views about the effects of these reductions on enrollment.
HHS did not set enrollment targets for 2018, but reported meeting its goal of enhancing specific aspects of consumer experience.
We recommended that HHS take steps to better manage its performance.
Healthcare.gov Enrollees, 2017 and 2018
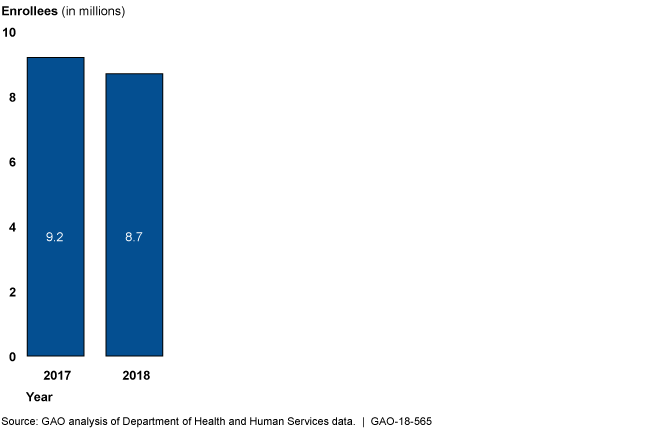
In 2017, there were 9.2 million healthcare.gov enrollees, and in 2018, there were 8.7 million.
Highlights
What GAO Found
About 8.7 million consumers in 39 states enrolled in individual market health insurance plans offered on the exchanges through healthcare.gov during the open enrollment period for 2018 coverage. This was 5 percent less than the 9.2 million who enrolled for 2017 and continued a decline in enrollment from a peak of 9.6 million in 2016. Among the 23 stakeholders we interviewed representing a range of perspectives, most reported that plan affordability played a major role in exchange enrollment—both attracting and detracting from enrollment. In 2018, total premiums increased more than expected, and, as a result, plans may have been less affordable for consumers, which likely detracted from enrollment. However, most consumers receive tax credits to reduce their premiums, and stakeholders reported that plans were often more affordable for these consumers because higher premiums resulted in larger tax credits, which likely aided exchange enrollment. Stakeholders had mixed opinions on the effects that other factors, such as the impact of reductions in federal advertising and the shortened open enrollment period, might have had on enrollment.
The Department of Health and Human Services (HHS), which manages healthcare.gov enrollment, reduced consumer outreach for the 2018 open enrollment period:
HHS spent 90 percent less on its advertising for 2018 ($10 million) compared to 2017 ($100 million). Officials told us that the agency's approach for 2018 was to focus on low-cost, high-performing forms of advertising.
HHS reduced funding by 42 percent for navigator organizations—which provide in-person enrollment assistance for consumers—spending $37 million in 2018 compared to $63 million in 2017 due to a shift in administration priorities. HHS allocated the funding using data that it acknowledged were not reliable in December 2016. The lack of quality data may affect HHS's ability to effectively manage the navigator program.
Unlike in prior years, HHS did not set any numeric targets related to 2018 total healthcare.gov enrollment; officials told us that they instead focused on enhancing the consumer experience for the open enrollment period. Setting numeric targets would allow HHS to monitor and evaluate its overall performance, a key aspect of federal internal controls. Further, while HHS reported meeting its goal of enhancing the consumer experience, such as by improving healthcare.gov availability, it did not measure aspects of the consumer experience it had identified as key in 2017, such as successful outreach events. Absent a more complete assessment, HHS may not be able to fully assess its progress toward its goal of enhancing the consumer experience and may miss opportunities to improve other aspects of the consumer experience.
Why GAO Did This Study
Since 2014, millions of consumers have purchased health insurance from the exchanges established by the Patient Protection and Affordable Care Act. Consumers can enroll in coverage during an annual open enrollment period. HHS and others conduct outreach during this period to encourage enrollment and ensure the exchanges' long-term stability. HHS announced changes to its 2018 outreach, prompting concerns that fewer could enroll, potentially harming the exchanges' stability.
GAO was asked to examine outreach and enrollment for the exchanges using healthcare.gov. This report addresses (1) 2018 open enrollment outcomes and any factors that may have affected these outcomes, (2) HHS's outreach efforts for 2018, and (3) HHS's 2018 enrollment goals. GAO reviewed HHS documents and data on 2018 open enrollment results and outreach. GAO also interviewed officials from HHS and 23 stakeholders representing a range of perspectives, including those from 4 navigator organizations, 3 issuers, and 6 insurance departments, to obtain their non-generalizable views on factors that likely affected 2018 enrollment.
Recommendations
GAO is making three recommendations to HHS, including that it ensure the data it uses for determining navigator organization awards are accurate, set numeric enrollment targets, and assess other aspects of the consumer experience. HHS agreed with two recommendations, but disagreed with the need to set numeric targets. GAO maintains that such action is important.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Department of Health and Human Services | The Secretary of HHS should ensure that the approach and data it uses for determining navigator award amounts accurately and appropriately reflect navigator organization performance, for example, by 1. providing clear guidance to navigator organizations on performance goals and other information they must report to HHS that will affect their future awards, 2. ensuring that the fields used to capture the information are functioning properly, and 3. assessing the effect of its current approach to funding navigator organizations to ensure that it is consistent with the agency's objectives. (Recommendation 1) |
HHS concurred with this recommendation and since our report was released, modified the formula it uses to determine navigator award amounts. Specifically, for the 2019 and 2020-2021 award periods, HHS largely based navigator awards on the size of the remaining eligible uninsured population in each state using the federally facilitated exchanges. In addition, HHS notified navigator organizations that future funding may be linked to navigators' self-identified performance goals and their ability to meet those goals. HHS has also taken several steps to improve the accuracy of the information it gathers with respect to navigator performance. For example, in September 2019, HHS reported expanding the training that it provides to navigators with respect to performance information they are required to submit. HHS also reported updating the healthcare.gov application to hold multiple navigator and agent/broker identification numbers.
|
| Department of Health and Human Services | The Secretary of HHS should establish numeric enrollment targets for healthcare.gov, to ensure it can monitor its performance with respect to its objectives. (Recommendation 2) |
CMS concurred with this recommendation and provided documentation showing that it had set and exceeded numeric enrollment targets for three consecutive fiscal years, and had continued setting targets for future years.
|
| Department of Health and Human Services | Should the agency continue to focus on enhancing the consumer experience as a goal for the program, the Secretary of HHS should assess other aspects of the consumer experience, such as those it previously identified as key, to ensure it has quality information to achieve its goal. (Recommendation 3) |
HHS initially concurred with our recommendation and reported examining ways to enhance the consumer experience as a goal for the program. In June 2021, HHS reported that it did not agree with the recommendation. In March 2024, HHS reported that it now concurs with the recommendation and is dedicated to providing a positive consumer experience. It noted that CMS recently updated its application and eligibility determination notice to prioritize the consumer experience, and has significantly increased its investment in consumer outreach, including through the use of in-person assistance programs. HHS also reported that CMS now regularly reviews consumer experience and examines call center satisfaction. HHS identified factors that have led to measurably different enrollment results, including a combination of greater affordability due to the Inflation Reduction Act, robust plan options, an improved consumer experience, and large-scale outreach and enrollment assistance. HHS also provided a list of its revised enrollment goals for the program through fiscal year 2026, and noted how it plans to assess the consumer experience in the future.
|
