Medicaid Assisted Living Services: Improved Federal Oversight of Beneficiary Health and Welfare is Needed
Fast Facts
Older people and people with disabilities receiving Medicaid assisted living services—over 330,000 in 2014—can be vulnerable to abuse, neglect or exploitation. The Centers for Medicare & Medicaid Services oversees how states monitor such incidents, but its guidance has been unclear.
More than half of the 48 states providing these services couldn’t tell us the number or nature of critical incidents in assisted living facilities. In addition, states may not be monitoring things you might expect them to. For example, 3 states don’t monitor unexpected or unexplained deaths.
We recommended that CMS take steps to improve state reporting.
Types of Incidents in Assisted Living Facility Services Monitored by 48 States in 2014
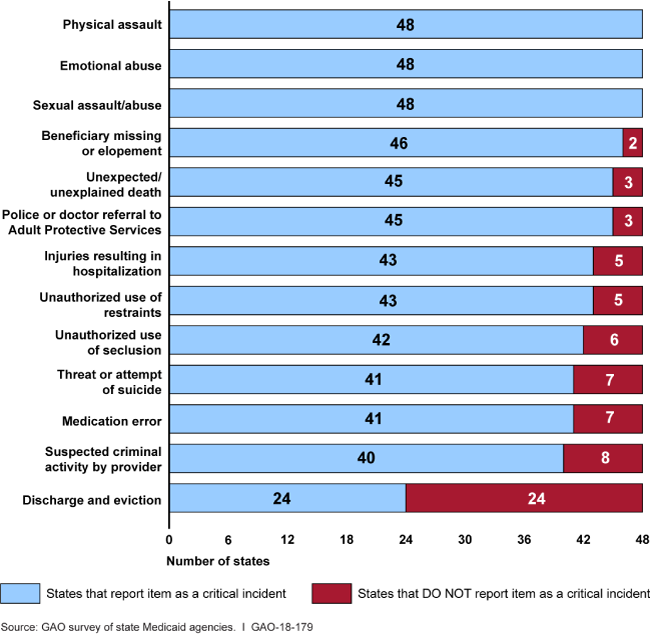
Graph showing types of incidents and numbers of states that defined or did not define them as critical.
Highlights
What GAO Found
State Medicaid agencies in 48 states that covered assisted living services reported spending more than $10 billion (federal and state) on assisted living services in 2014. These 48 states reported covering these services for more than 330,000 beneficiaries through more than 130 different programs. Most programs were operated under Medicaid waivers that allow states to target certain populations, limit enrollment, or restrict services to certain geographic areas.
With respect to oversight of their largest assisted living programs, state Medicaid agencies reported varied approaches to overseeing beneficiary health and welfare, particularly in how they monitored critical incidents involving beneficiaries receiving assisted living services. State Medicaid agencies are required to protect beneficiary health and welfare and operate systems to monitor for critical incidents—cases of potential or actual harm to beneficiaries such as abuse, neglect, or exploitation.
Twenty-six state Medicaid agencies could not report to GAO the number of critical incidents that occurred in assisted living facilities, citing reasons including the inability to track incidents by provider type (9 states), lack of a system to collect critical incidents (9 states), and lack of a system that could identify Medicaid beneficiaries (5 states).
State Medicaid agencies varied in what types of critical incidents they monitored. All states identified physical, emotional, or sexual abuse as a critical incident. A number of states did not identify other incidents that may indicate potential harm or neglect such as medication errors (7 states) and unexplained death (3 states).
State Medicaid agencies varied in whether they made information on critical incidents and other key information available to the public. Thirty-four states made critical incident information available to the public by phone, website, or in person, while another 14 states did not have such information available at all.
Oversight of state monitoring of assisted living services by the Centers for Medicare & Medicaid Services (CMS), an agency within the Department of Health and Human Services (HHS), is limited by gaps in state reporting. States are required to annually report to CMS information on deficiencies affecting beneficiary health and welfare for the most common program used to provide assisted living services. However, states have latitude in what they consider a deficiency. States also must describe their systems for monitoring critical incidents, but CMS does not require states to annually report data from their systems. Under federal internal control standards, agencies should have processes to identify information needed to achieve objectives and address risk. Without clear guidance on reportable deficiencies and no requirement to report critical incidents, CMS may be unaware of problems. For example, CMS found, after an in-depth review in one selected state seeking to renew its program, that the state lacked an effective system for assuring beneficiary health and welfare, including reporting insufficient information on the number of unexpected or suspicious beneficiary deaths. The state had not reported any deficiencies in annual reports submitted to CMS in 5 prior years.
Why GAO Did This Study
The number of individuals receiving long term care services from Medicaid in community residential settings is expected to grow. These settings, which include assisted living facilities, provide a range of services that allow aged and disabled beneficiaries, who might otherwise require nursing home care, to remain in the community.
State Medicaid programs and CMS, the federal agency responsible for overseeing the state programs, share responsibility for ensuring that beneficiaries' health and welfare is protected. GAO was asked to examine state and federal oversight of assisted living services in Medicaid. This report (1) describes state spending on and coverage of these services, (2) describes how state Medicaid agencies oversee the health and welfare of beneficiaries in these settings, and (3) examines the extent that CMS oversees state Medicaid agency monitoring of assisted living services.
GAO surveyed all state Medicaid agencies and interviewed officials in a nongeneralizeable sample of three states with varied oversight processes for their assisted living programs. GAO reviewed regulations and guidance, and interviewed CMS officials.
Recommendations
GAO recommendations to CMS include clarifying state requirements for reporting program deficiencies and requiring annual reporting of critical incidents. HHS concurred with GAO's recommendations to clarify deficiency reporting and stated that it would consider annual reporting requirements for critical incidents after completing an ongoing review.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should provide guidance and clarify requirements regarding the monitoring and reporting of deficiencies that states using home and community-based services (HCBS) waivers are required to report on their annual reports. (Recommendation 1) |
CMS concurred with this recommendation and indicated the agency would provide guidance and clarify requirements regarding the monitoring and reporting of deficiencies in states' annual HCBS reports. As of January 2025, CMS reported that the agency had released an updated technical guide for the annual HCBS reports. The updated technical guide specifies that states need to provide data for each performance measure and include information about how any identified deficiencies will be remediated.
|
| Centers for Medicare & Medicaid Services |
Priority Rec.
The Administrator of CMS should establish standard Medicaid reporting requirements for all states to annually report key information on critical incidents, considering, at a minimum, the type of critical incidents involving Medicaid beneficiaries, and the type of residential facilities, including assisted living facilities, where critical incidents occurred. (Recommendation 2) |
HHS neither agreed nor disagreed with this recommendation. As of January 2023, CMS had provided states with technical assistance on critical incident reporting, including providing training and an optional incident reporting template. CMS released a final rule in April 2024 that included provisions to standardize critical incident oversight, including requirements to report data to CMS. In January 2025, CMS reported that the agency was developing guidance on the reporting requirements. As of March 2026, there has been no additional action reported by the agency. Once the reporting is in effect, GAO will review and determine whether the recommendation has been implemented.
|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should ensure that all states submit annual reports for HCBS waivers on time as required. (Recommendation 3) |
CMS concurred with this recommendation and stated that it will review and update its communications with states to reaffirm reporting requirements and ensure that all HCBS annual reports are submitted on time. As of October 2025, CMS reported that the agency conducts outreach to states to remind them of upcoming due dates for the annual reports. CMS also publishes a measure in its Medicaid and CHIP scorecard that reports on the timeliness of states' annual HCBS report submissions and takes into account approved flexibilities to submit at a later date granted due to the COVID-19 public health emergency. The data for calendar year 2024 indicate a similar volume of late state reports as when we issued this report. Once CMS has implemented critical incident reporting requirements, which could serve as an alternative source of oversight information, or improves on its measure of timeliness for the annual HCBS waiver reports, GAO will reassess whether the recommendation has been implemented.
|
