Medicare: CMS Fraud Prevention System Uses Claims Analysis to Address Fraud
Fast Facts
The Centers for Medicare & Medicaid Services has an IT system—the Fraud Prevention System— that analyzes claims to identify health care providers with suspect billing patterns. Program integrity contractors get leads from the system to pursue fraud investigations.
We found that the system accounted for about 20 percent of CMS's fraud investigations in fiscal years 2015 and 2016. It also helped the contractors identify leads and triage them faster (shown below).
The system also uses automated controls that identify payments associated with potential fraud and deny claims that violate Medicare rules or policies before the claims are paid.
Program Integrity Contractor Investigation Process
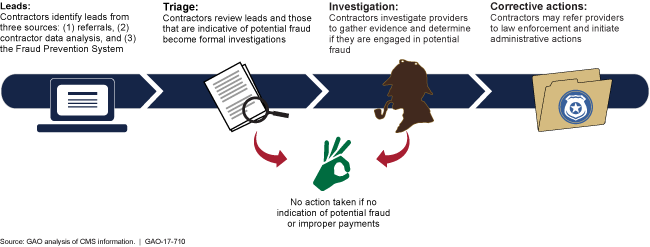
Graphic showing leads followed by triage, then investigation and ending in corrective actions
Highlights
What GAO Found
Investigations initiated or supported by the Centers for Medicare & Medicaid Services' (CMS) Fraud Prevention System (FPS)—a data analytic system—led to corrective actions against providers and generated savings. For example, in fiscal year 2016, CMS reported that 90 providers had their payments suspended because of investigations initiated or supported by FPS, which resulted in an estimated $6.7 million in savings. In fiscal year 2016, 22 percent of Medicare fraud investigations conducted by CMS program integrity contractors were based on leads generated by FPS analysis of Medicare claims data. Officials representing Medicare's program integrity contractors told GAO that FPS helps speed up certain investigation processes, such as identifying and triaging suspect providers for investigation. However, the officials said that once an investigation is initiated, FPS has generally not sped up the process for investigating and gathering evidence against suspect providers. CMS has not tracked data to assess the extent to which FPS has affected the timeliness of contractor investigation processes. However, CMS is implementing a new information technology system that tracks such data, and officials said that they plan to use the data to assess FPS's effect on timeliness.
FPS denies individual claims for payment that violate Medicare rules or policies through prepayment edits—automated controls that compare claims against Medicare requirements in order to approve or deny claims. FPS prepayment edits specifically target payments associated with potential fraud. For example, an FPS edit denies physician claims that improperly increase payments by misidentifying the place that the service was rendered, which helped address a payment vulnerability associated with millions in overpayments. FPS edits do not analyze individual claims to automatically deny them based on risk alone or the likelihood that they are fraudulent without further investigation. As of May 2017, CMS had implemented 24 edits in FPS. CMS reported that FPS edits denied nearly 324,000 claims and saved more than $20.4 million in fiscal year 2016.
The Healthcare Fraud Prevention Partnership (HFPP) is a public-private partnership that began in 2012 with the aim of facilitating collaboration among health care payers to address health care fraud. The HFPP had 79 participants as of June 2017. Participants, including CMS officials, stated that sharing data and information within HFPP has been useful to their efforts to address health care fraud. HFPP conducts studies that pool and analyze multiple payers' claims data to identify providers with patterns of suspect billing across payers. Participants reported that HFPP's studies helped them to identify and take action against potentially fraudulent providers and payment vulnerabilities of which they might not otherwise have been aware. For example, one study identified providers who were cumulatively billing multiple payers for more services than could reasonably be rendered in a single day. Participants also stated that HFPP has fostered both formal and informal information sharing among payers.
The Department of Health and Human Services provided technical comments on a draft of this report, which GAO incorporated as appropriate.
Why GAO Did This Study
CMS analyzes Medicare fee-for-service claims data to further its program integrity activities. In 2011, CMS implemented a data analytic system called FPS to develop leads for fraud investigations conducted by CMS program integrity contractors and to deny improper payments. In developing leads, FPS is intended to help CMS avoid improper payment costs by enabling quicker investigations and more timely corrective actions. Additionally, in 2012, CMS helped establish the HFPP to collaborate with other health care payers to address health care fraud. One of the key activities of the HFPP is to analyze claims data that are pooled from multiple payers, including private payers and Medicare.
GAO was asked to review CMS's use of FPS and the activities of the HFPP. This report examines 1) CMS's use of FPS to identify and investigate providers suspected of potential fraud, 2) the types of payments that have been denied by FPS, and 3) HFPP efforts to further CMS's and payers' ability to address health care fraud. GAO reviewed CMS documents, including reports to Congress on FPS, contractor statements of work, and information technology system user guides, and obtained fiscal year 2015 and 2016 data on FPS fraud investigations and claim denials. GAO also interviewed CMS officials and CMS program integrity contractors regarding how they use FPS, and a non-generalizable selection of HFPP participants regarding information and data sharing practices, and anti-fraud collaboration efforts.
For more information, contact Kathleen M. King at (202) 512-7114 or kingk@gao.gov.
