Medicaid Managed Care: CMS Should Improve Oversight of Access and Quality in States' Long-Term Services and Supports Programs
Fast Facts
Medicaid beneficiaries who need long-term care can get it in their homes, community settings, or an institution such as a nursing home. Many states contract with managed care organizations to provide this care.
The 6 states we reviewed used various methods (e.g., beneficiary surveys) to monitor access and quality in managed long-term care programs. However, the Centers for Medicare & Medicaid Services did not always require the states to report information it needs for oversight, such as beneficiary concerns or whether there are enough providers.
We recommended that CMS improve its oversight.
States with Current or Planned Managed Long-term Services and Supports Programs, May 2017
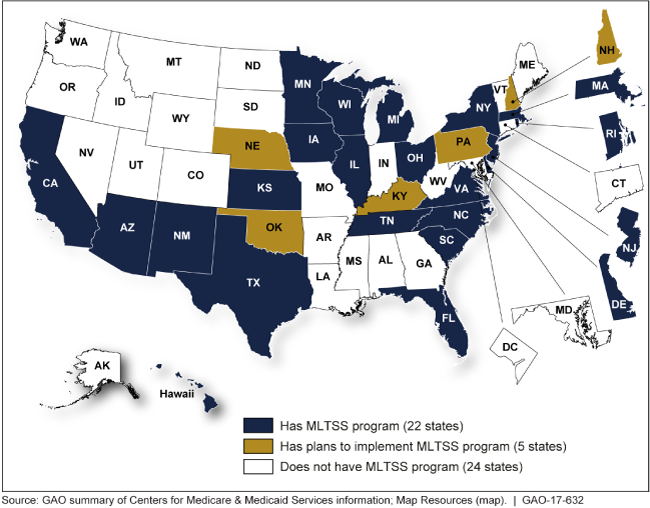
A map of the United States showing that 27 states have or will have these programs, as of May 2017.
Highlights
What GAO Found
In Medicaid, long-term services and supports are designed to promote the ability of beneficiaries with physical, cognitive, or mental disabilities or conditions to live or work in the setting of their choice, which can be in home or community settings, or in an institution such as a nursing facility. States are increasingly delivering such services through managed care, known as managed long-term services and supports (MLTSS). In MLTSS, as with most Medicaid managed care programs, states contract with managed care organizations (MCO) to provide a specific set of covered services to beneficiaries in return for one fixed periodic payment per beneficiary. In addition, beneficiaries have the right to appeal an MCO decision to reduce, terminate, or deny their benefits, or file a grievance with an MCO regarding concerns about their care.
The six states GAO reviewed—Arizona, Delaware, Kansas, Minnesota, Tennessee, and Texas—used a range of methods for monitoring access and quality in MLTSS programs. To oversee beneficiaries' care, GAO found that states used—to varying levels—external quality reviews, beneficiary surveys, stakeholder meetings, and beneficiary appeals and grievances data. For example, while all six states used external quality reviews and beneficiary surveys, GAO found that states varied in the extent to which—and how—they used appeals and grievances data to monitor beneficiaries' concerns about quality and access in their MLTSS programs.
The Centers for Medicare & Medicaid Services (CMS)—the federal agency responsible for overseeing Medicaid—did not always require the six selected states to report the information needed to monitor access and quality in MLTSS programs. CMS primarily relied on its reviews of state-submitted reports to monitor MLTSS programs for compliance with federal regulations and state-specific reporting requirements, and what states are required to report to CMS can vary by state. Although CMS highlighted certain elements that it deemed essential to developing and maintaining high quality MLTSS programs in its 2013 guidance, GAO found that CMS did not require all selected states to report on these elements—namely, provider network adequacy; critical incidents, which are events that may cause abuse, neglect or exploitation of beneficiaries; and appeals and grievances. CMS did not require three of the six states that GAO reviewed to regularly report on network adequacy or provide summaries of critical incidents. Further, although CMS requires all selected states to report on their quality assurance efforts, GAO found that states often report general descriptions of their planned and ongoing quality assurance activities for MLTSS or their entire comprehensive managed care programs. Consequently, state reporting did not always provide CMS with information needed to assess state oversight of key elements. Gaps in reporting requirements may mean that CMS does not always have information needed to monitor key aspects of MLTSS access and quality among selected states and it may not be able to reliably detect state or MCO practices that do not meet CMS's guidance.
Why GAO Did This Study
Twenty-two states use MLTSS programs to provide care for Medicaid beneficiaries who need long-term support. Using managed care to deliver long-term services and supports can be a strategy for states to expand home- and community-based care, which many beneficiaries prefer, and to lower costs. However, given the potential vulnerability and needs of beneficiaries in these programs, oversight is crucial to ensure their access to quality care.
GAO was asked to review states' implementation and CMS's oversight of MLTSS programs. In this report, GAO (1) described how selected states monitored MLTSS access and quality, and (2) examined the extent to which CMS oversees MLTSS access and quality in selected states.
GAO reviewed federal regulations, guidance, and internal control standards. For six states selected for variation in location, program size and duration, and other factors, GAO reviewed reporting requirements, reports to CMS, and other documents. GAO also reviewed data from these states on beneficiary appeals and grievances from 2013 through 2015—the most recent data available—and interviewed state and CMS officials.
Recommendations
GAO recommends that CMS take steps to identify and obtain information to oversee key aspects of MLTSS access and quality, including network adequacy, critical incidents, and appeals and grievances. HHS concurred with GAO's recommendation.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Centers for Medicare & Medicaid Services | To improve CMS's oversight of states' MLTSS programs, the Administrator of CMS should take steps to identify and obtain key information needed to oversee states' efforts to monitor beneficiary access to quality services, including, at a minimum, obtaining information specific to network adequacy, critical incidents, and appeals and grievances. |
In June 2021, CMS issued guidance to states that triggered the requirement for states to submit annual reports on their Medicaid managed care programs. The guidance included a reporting template. The template indicates that the state annual reports are to include information on health plan performance in providing LTSS. Among other things, states are required to report data for each participating health plan on appeals, grievances, and critical incidents for LTSS users and plan performance on measures of network adequacy. CMS officials told us that they expect these annual reports to provide more consistent and comprehensive information from states on quality and access in managed care broadly, and LTSS specifically.
|
