Health Care: Telehealth and Remote Patient Monitoring Use in Medicare and Selected Federal Programs
Fast Facts
Does Medicare pay when beneficiaries use two-way video visits to get care from their doctors?
It depends. Medicare pays for some two-way video visits—referred to as "telehealth"—if the patients connect from rural health facilities. Generally, Medicare doesn’t pay for telehealth in urban facilities or in the patient's home or office.
We talked to some health care associations, who believe that telehealth has the potential to maintain or improve quality of care and said that these rules create barriers to using telehealth.
Medicare is testing new ways to provide health care that allow telehealth coverage regardless of location.
Example of Telehealth Use with Medicare
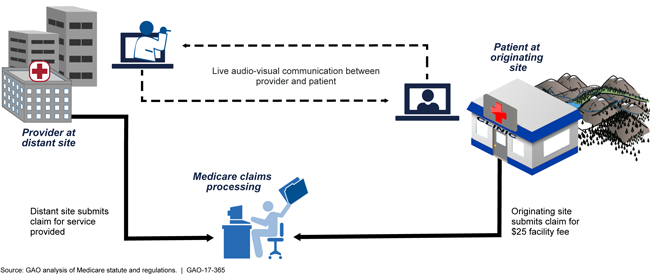
Illustrated flow chart of a telehealth session and how Medicare handles the related claims.
Highlights
What GAO Found
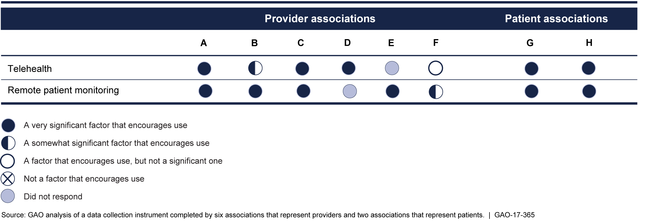
Selected associations representing providers and patients most often cited the potential to improve or maintain quality of care as a significant factor that encourages the use of telehealth (providing clinical care remotely by two-way video) and remote patient monitoring (monitoring of patients outside of conventional settings) in Medicare. For example, according to officials from a provider association, telehealth can improve patient outcomes by facilitating follow-up care, while remote patient monitoring is helpful for treating patients with chronic diseases. With regard to factors that create barriers, the selected associations most often cited concerns over payment and coverage restrictions. For example, officials from a provider association noted that Medicare telehealth coverage restrictions limit the geographic and practice settings in which beneficiaries may receive services. While not indicating how significant these factors are to Medicare, officials with a payer association told GAO that they considered these factors—also identified by the provider and patient associations—as either encouraging use or creating barriers to the use of telehealth and remote patient monitoring.
Significance of Improving or Maintaining Quality of Care as a Factor that Encourages the Use of Telehealth and Remote Patient Monitoring in Medicare
Medicare models, demonstrations, and a new payment program have the potential to expand the use of telehealth and remote patient monitoring. The Centers for Medicare & Medicaid Services, an agency within the Department of Health and Human Services (HHS), supports eight models and demonstrations in which certain Medicare telehealth requirements have been waived, such as requirements for the locations and facility types where beneficiaries can receive telehealth services. For example, the waivers allow beneficiaries to access telehealth in urban areas, or from their homes. Additionally, the use of telehealth and remote patient monitoring in Medicare may change depending on how many clinicians use them as a way to achieve the goals of the new Merit-based Incentive Payment System, which—starting in 2017—will pay clinicians based on quality and resource use, among other things. Under this payment program, clinicians can use telehealth and, in some instances, remote patient monitoring, to help meet the payment program's performance criteria. For example, clinicians could use telehealth to coordinate care or use remote patient monitoring to remotely gather information to determine a patient's proper dose of medication.
Why GAO Did This Study
Telehealth and remote patient monitoring can provide alternatives to health care provided in person at a physician's office, particularly for patients who cannot easily travel long distances for care. Medicare pays for some telehealth services that are subject to statutory and regulatory requirements, such as requiring the patient be present at an originating site like a rural health clinic.
The Medicare Access and CHIP Reauthorization Act of 2015 includes a provision for GAO to study telehealth and remote patient monitoring. Among other reporting objectives, this report reviews (1) the factors that associations identified as affecting the use of telehealth and remote patient monitoring in Medicare and (2) emerging payment and delivery models that could affect the potential use of telehealth and remote patient monitoring in Medicare.
GAO reviewed agency documents and regulations and interviewed agency officials. GAO also selected nine general and medical specialty associations with expertise and interest in telehealth or remote patient monitoring—six provider, two patient, and one payer association—based on a review of relevant documents and literature and through background interviews. GAO interviewed representatives from each of the associations and collected information from the provider and patient associations through a data collection instrument.
GAO provided a draft of this report to HHS. In response, HHS provided technical comments, which were incorporated as appropriate.
For more information, contact Carolyn L. Yocom at (202) 512-7114 or Yocomc@gao.gov.
