Medicare Advantage: CMS Should Fully Develop Plans for Encounter Data and Assess Data Quality before Use
Highlights
What GAO Found
The Centers for Medicare & Medicaid Services (CMS) is collecting Medicare Advantage (MA) encounter data—information on the services and items furnished to enrollees—that are more comprehensive than the beneficiary diagnosis data the agency currently uses to risk adjust capitated payments to MA organizations (MAO). CMS, an agency within the Department of Health and Human Services (HHS), makes these adjustments to reflect the expected health care costs of MA enrollees. Encounter data have many more elements—including procedure codes and provider payments—from a wider range of provider types—such as home health agencies and skilled nursing facilities—thus expanding the scope of sources for diagnosis and other information.
CMS has not fully developed plans for using MA encounter data. The agency announced that it will begin using diagnoses from both encounter data and the data it currently collects for risk adjustment to determine payments to MAOs in 2015. However, CMS has not established time frames or specific plans to use encounter data for other potential purposes.
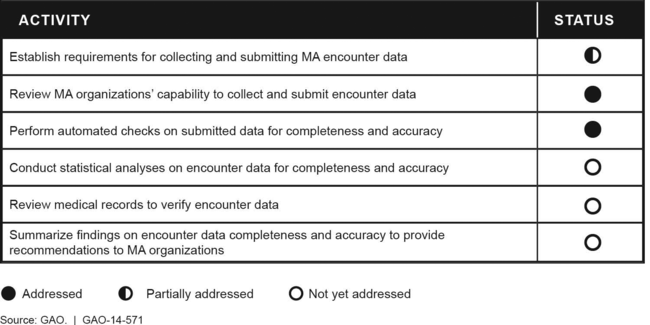
CMS has taken some, but not yet all, appropriate actions to ensure that MA encounter data are complete and accurate. (See figure.) The agency has established timeliness and frequency requirements for data submission, but has not yet developed requirements for completeness and accuracy. Also, the agency has certified nearly all MAOs to transmit encounter data. Although CMS performs automated checks to determine whether key data elements are completed and values are reasonable, it has not yet performed statistical analyses that could detect more complex data validity issues. For example, CMS has not yet generated basic statistics from the data by demographic group or provider type to identify inconsistencies or gaps in the data. Also, it has not yet reviewed medical records to verify diagnoses and services listed in encounter data or reported what it has learned about data quality to MAOs. Agency officials told GAO they intend to perform these additional quality assurance activities but have not established time frames to do so.
Status of the Centers for Medicare & Medicaid Services' Activities to Validate Medicare Advantage (MA) Encounter Data, May 2014
Why GAO Did This Study
Medicare Advantage—the private plan alternative to the traditional Medicare program—provides health care for nearly 15.5 million enrollees, about 30 percent of all Medicare beneficiaries. After a multiyear rollout, CMS began collecting encounter data in January 2012. GAO was asked to review CMS's plans for using MA encounter data and its efforts to validate the data's quality.
This report examines (1) how the scope of MA encounter data compare with CMS's current risk adjustment data, (2) the extent to which CMS has specified plans and time frames to use encounter data for risk adjustment and other purposes, and (3) the extent to which CMS has taken appropriate steps to ensure MA encounter data's completeness and accuracy. In addition to reviewing laws, regulations, and guidance on MA encounter data collection and reporting, GAO interviewed CMS officials and representatives of MAOs. GAO also compared CMS's activities to the protocol CMS developed to validate Medicaid encounter data—comparable data collected and submitted by entities similar to MAOs.
Recommendations
CMS should establish specific plans for using MA encounter data and thoroughly assess data completeness and accuracy before using the data to risk adjust payments or for other purposes. While in general agreement, HHS did not specify a date by which CMS will develop plans for all authorized uses of encounter data and did not commit to completing data validation before using the data for risk adjustment in 2015.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Centers for Medicare & Medicaid Services |
Priority Rec.
To ensure that MA encounter data are of sufficient quality for their intended purposes, the Administrator of CMS should establish specific plans and time frames for using the data for all intended purposes in addition to risk adjusting payments to MAOs. |
HHS generally agreed with this recommendation. As of September 2022, CMS is using MA encounter data in various ways other than risk adjustment. For example, CMS uses MA encounter data to obtain diagnoses for Part D Medicaid Adherence measures. CMS has also used MA encounter data as part of evaluating the first 3 years of MA's Value-Based Insurance Design Model--health insurers' efforts to structure health plan elements to encourage enrollees with chronic conditions to use particularly beneficial services. In addition, CMS has begun using MA encounter data for program integrity purposes. For example, a program integrity contractor uses MA encounter data to identify providers with patterns of encounters that may be indicative of fraud, waste, and abuse. In light of these additional uses of MA encounter data, we are closing this recommendation as implemented.
|
| Centers for Medicare & Medicaid Services |
Priority Rec.
To ensure that MA encounter data are of sufficient quality for their intended purposes, the Administrator of CMS should complete all the steps necessary to validate the data, including performing statistical analyses, reviewing medical records, and providing MAOs with summary reports on CMS's findings, before using the data to risk adjust payments or for other intended purposes. |
HHS generally agreed with this recommendation. As of February 2025, CMS has made progress in examining the completeness and accuracy of Medicare Advantage encounter data, but an additional step remains to fully validate these data. Specifically, CMS has not demonstrated that it verifies encounter data by systematically reviewing medical records in a timely manner. However, CMS partially implemented our recommendation by taking other key steps to validate these data. For example, CMS has established some performance metrics for MA encounter data completeness and accuracy and further developed associated analyses. Specifically, the agency continues to conduct automated checks for data consistency and validity as part of accepting data. Also, MAOs receive reports regarding the acceptance or rejection of data they submitted. Further, the agency conducts various analyses of encounter data completeness and accuracy for internal purposes. Based on these analyses, the agency identifies MAOs with persistent rates of rejected encounter data and may contact them to understand reasons causing high rejection rates when submitting data. CMS has also developed standards for submission performance based on meeting eight thresholds and sends reports to MAOs indicating whether they are meeting these thresholds. These efforts are consistent with the requirements specified in the agency's protocol for assessing the completeness and accuracy of Medicaid data. Until CMS fully validates the completeness and accuracy of MA encounter data, the soundness of adjustments to payments to MA organizations remains unsubstantiated.
|
