Medicare Advantage: Plans Generally Offered Some Supplemental Benefits, but CMS Has Limited Data on Utilization
Fast Facts
About half of Medicare users are enrolled in Medicare Advantage (MA), private plans that offer the same benefits covered under Original Medicare and may offer additional benefits, such as dental or vision. In recent years, MA plans could offer new types of supplemental benefits, like in-home support services.
But are plans offering additional benefits, and are people using them? We analyzed data for 3,893 plans across the nation to find out.
About a third offered at least one of the new types of additional benefits. But plans' reporting of people's use of additional benefits was incomplete. We recommended ways to better collect this data.

Highlights
What GAO Found
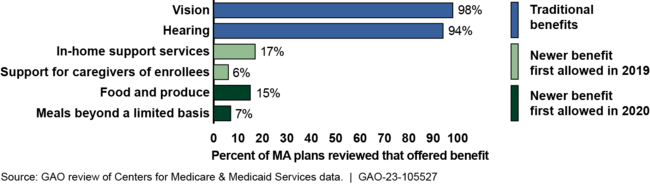
Under Medicare Advantage (MA), a private plan option in Medicare, plans can offer supplemental benefits not covered under Original Medicare. Supplemental benefits have long included traditional health-related benefits. In 2022, all but one plan reviewed by GAO offered at least one such benefit; the most common were vision and hearing. (See figure.) MA plans can also offer two newer types of benefits. First, starting in 2019, plans could offer benefits intended to reduce avoidable health care use, among other things. Second, starting in 2020, plans could offer benefits with a reasonable expectation of improving or maintaining the health or function of chronically ill enrollees. In 2022, about one-third of plans reviewed offered at least one of the newer types of benefits; the most common were in-home support services and food and produce.
Most Common Supplemental Benefits, by Type, Offered by Medicare Advantage (MA) Plans Reviewed, 2022
MA plans are required to submit detailed, service-level utilization data to the Centers for Medicare & Medicaid Services (CMS), the agency that oversees MA. These data—known as encounter data—must include supplemental benefits to the extent required by CMS. However, GAO found that information submitted by plans on enrollees' use of supplemental benefits is limited for two reasons:
- CMS guidance on encounter data does not specifically mention the submission of such data for supplemental benefits, although it says plans must submit encounter data for each benefit provided to an enrollee. CMS officials told GAO that the inclusion of supplemental benefits in this requirement is clear, noting the guidance does not differentiate between supplemental and Original Medicare benefits. However, officials from three MA organizations told GAO they are not required to submit encounter data for some or all supplemental benefits and therefore do not do so.
- Officials from CMS and two MA organizations told GAO there are challenges collecting and submitting encounter data for certain supplemental benefits. For example, officials said there is no procedure code for some of the newer supplemental benefits, such as food and produce.
As of October 2022, CMS was in the early stages of assessing the completeness of the encounter data for supplemental benefits and identifying options for collecting enrollee utilization data for the newer benefits but did not have a workplan or timeline for next steps. More complete information on enrollees' use of supplemental benefits would put CMS in a stronger position to ensure the benefits effectively support the health and social needs of enrollees.
Why GAO Did This Study
MA plans decide which, if any, supplemental benefits to offer. These benefits may be attractive to Medicare beneficiaries, but little is known about their use.
The Bipartisan Budget Act of 2018 includes a provision for GAO to review supplemental benefits. Among other things, this report describes the supplemental benefits offered by MA plans in 2022 and examines the information that CMS has on enrollees' use of supplemental benefits and their effects on enrollees' health and function.
GAO analyzed plan benefit data for 3,893 MA plans in the 50 states and District of Columbia. GAO excluded certain plans, such as plans participating in the Value-Based Insurance Design Model and employer plans, to ensure comparability between plans. GAO also reviewed CMS regulations and guidance and interviewed officials from CMS and six MA organizations selected based on enrollment, geographic coverage, and other factors.
Recommendations
GAO is making two recommendations to CMS: (1) clarify guidance on the extent to which encounter data submissions must include data on the utilization of supplemental benefits and (2) address circumstances where submitting encounter data for supplemental benefits is challenging for MA plans, such as when a given benefit lacks an applicable procedure code. The Department of Health and Human Services concurred with the recommendations.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should clarify guidance to MA plans on the extent to which encounter data submissions must include data on the utilization of supplemental benefits. (Recommendation 1) |
In February 2024, CMS released guidance clarifying that MA plans are required to submit encounter data for all supplemental benefits provided to their enrollees. The guidance explains that federal regulations requiring MA plans to submit encounter data for each benefit provided to a Medicare enrollee applies not only to Medicare Part A and B covered items and services, but also to supplemental benefits provided to MA enrollees. MA plans are required to submit these data starting with supplemental benefits provided in 2024 in accordance with updated instructions provided in the guidance.
|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should take actions to address circumstances where submitting encounter data for supplemental benefits is challenging for MA plans, such as when a given benefit lacks an applicable procedure code. Such actions may include the creation of new procedure codes or a new data submission format. (Recommendation 2) |
In February 2024, CMS announced changes to its MA Encounter Data System, including actions it had taken to address challenges MA plans have had submitting encounter data for certain supplemental benefits. For example, to address the submission of encounter data for supplemental benefits for which diagnosis, procedure, or revenue codes do not exist, CMS created default codes and provided instructions to plans on how to use these default codes to submit encounter data. In other circumstances, CMS said it expects MA plans to obtain the specific codes from the provider or vendor. CMS also provided instructions for how to submit encounter data for benefits that have varied payment approaches, such as benefits that are paid on an annual or quarterly basis, which had been a challenge for plans. In addition, CMS developed a new supplemental benefits indicator and supplemental benefit category codes that align with categories used in the plans' bids that plans must use when submitting their encounter data. CMS said that use of this indicator will allow it to identify supplemental benefits in the encounter data. MA plans are required to submit these data starting with supplemental benefits provided in 2024 in accordance with the updated instructions.
|
