Medicare Part B: Payments and Use for Selected New, High-Cost Drugs
Fast Facts
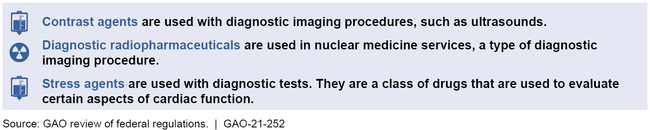
Hospital outpatient departments use certain drugs for surgical or diagnostic procedures. An example is a drug to more clearly view organs during an ultrasound.
If those drugs are new and cost more, Medicare pays hospitals for the procedure and makes an additional "pass-through" payment for the drug, for the first 2 to 3 years. After pass-through payments expire, Medicare pays for the drug as part of a single payment for the procedure.
We found
hospitals used some drugs more when the drugs were eligible for pass-through payments
for 6 of the 7 drugs we reviewed, Medicare paid less for the drug and procedure after pass-through payments expired

Highlights
What GAO Found
Hospital outpatient departments perform a wide range of procedures, including diagnostic and surgical procedures, which may use drugs that Medicare considers to function as supplies. If the drug is new, and its cost is high relative to Medicare's payment for the procedure, then hospitals can receive a separate “pass-through” payment for the drug in addition to Medicare's payment for the procedure. These pass-through payments are in effect for 2 to 3 years. When the pass-through payments expire, Medicare no longer pays separately for the drug, and payment for the drug is “packaged” with the payment for the related procedure. The payment rate for the procedure does not vary by whether or not the drug is used. Medicare intends this payment rate to be an incentive for hospitals to furnish services efficiently, such as using the most cost-efficient items that meet the patient's needs.
Examples of Types of Drugs that Medicare Considers to Function as Supplies
GAO's analysis of Medicare data showed that higher payments were associated with six of seven selected drugs when they were eligible for pass-through payments versus when their payments were packaged. For example, one drug used in cataract removal procedures was eligible for pass-through payments in 2017. That year, Medicare paid $1,824 for the procedure and $463 for the drug pass-through payment—a total payment of $2,287. If a hospital performed the same cataract removal procedure when the drug was packaged the following year, there was no longer a separate payment for the drug. Instead, Medicare paid $1,921 for the procedure whether or not the hospital used the drug.
Of the seven selected drugs, GAO also reviewed differences in use for four of them that did not have limitations on Medicare coverage during the time frame of GAO's analysis, such as coverage that was limited to certain clinical trials. GAO found that hospitals' use of three of the four drugs was lower when payments for the drugs were packaged. This was consistent with the financial incentives created by the payment system. In particular, given the lower total payment for the drug and procedure when the drug is packaged, hospitals may have a greater incentive to use a lower-cost alternative for the procedure. Hospitals' use of a fourth drug increased regardless of payment status. The financial incentives for that drug appeared minimal because the total payment for it and its related procedure was about the same when it was eligible for pass-through payments and when packaged. Other factors that can affect use of the drugs include the use of the drugs for certain populations and whether hospitals put the drugs on their formularies, which guide, in part, whether the drug is used at that hospital.
The Department of Health and Human Services reviewed a draft of this report and provided technical comments, which GAO incorporated as appropriate.
Why GAO Did This Study
Medicare makes “pass-through” payments under Medicare Part B when hospital outpatient departments use certain new, high-cost drugs. These temporary payments are in addition to Medicare's payments for the procedures using the drugs. They may help make the new drugs accessible for beneficiaries and also allow Medicare to collect information on the drugs' use and costs.
The Consolidated Appropriations Act, 2018 included a provision for GAO to review the effect of Medicare's policy for packaging high-cost drugs after their pass-through payments have expired. This report describes (1) the payments associated with selected high-cost drugs when eligible for pass-through payments versus when packaged, and (2) hospitals' use of those drugs when eligible for pass-through payments versus when packaged.
GAO reviewed federal regulations on pass-through payments and Medicare payment files for all seven drugs whose pass-through payments expired in 2017 or 2018 and that were subsequently packaged. All of these drugs met Medicare's definition for having a high cost relative to Medicare's payment rate for the procedure using the drug. GAO also reviewed Medicare claims data on the use of the drugs for 2017 through 2019 (the most recent available). To supplement this information, GAO also interviewed Medicare officials, as well officials from 11 organizations representing hospitals, physicians, and drug manufacturers, about payment rates, use, reporting, and clinical context for the drugs.
For more information, contact James Cosgrove at (202) 512-7114 or cosgrovej@gao.gov.