Railroad Retirement Board: Actions Needed to Improve the Effectiveness and Oversight of Continuing Disability Reviews
Highlights
What GAO Found
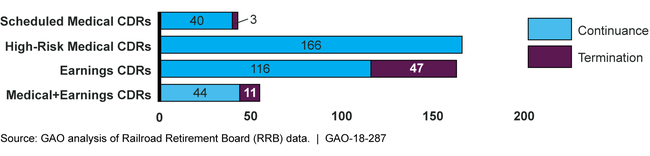
In fiscal years 2014-2016, the Railroad Retirement Board (RRB) completed continuing disability reviews (CDRs) of various types for 427 beneficiaries (see figure below), covering slightly more than 1 percent of the railroad workers who received disability benefits during that period. These reviews included:
Scheduled Medical Reviews –These are scheduled at different intervals depending on the likelihood of medical improvement. RRB data suggest that most beneficiaries are not subject to these CDRs because they are older than 54½, which RRB defines as the age at which they are unlikely to return to work. Of 43 medical CDRs that were scheduled, RRB identified 3 ineligible beneficiaries and 1 overpayment of about $28,000.
High-Risk Reviews – In fiscal year 2015, RRB began conducting medical CDRs on cases it considered to be at high risk for fraud. It completed 166 of these reviews in fiscal years 2015 and 2016, but none identified any ineligible beneficiaries or overpayments.
Earnings Reviews – During fiscal years 2014-2016, 163 earnings CDRs identified 47 ineligible beneficiaries and at least $970,550 in overpayments. However, RRB uses earnings information that can be up to 2 years old, thereby delaying the detection of ineligible beneficiaries and increasing the potential for lost federal dollars. Other federal agencies have access to a national federal database with more recent earnings data. Providing RRB access to these data would enable it to identify overpayments sooner.
Medical + Earnings Reviews – In some cases, RRB conducts both a medical and earnings CDR. RRB's data do not allow GAO to attribute the outcome to either type of CDR.
Continuing Disability Reviews (CDR) Completed by the Railroad Retirement Board for Fiscal Years 2014-2016, by Type and Outcome
RRB oversight has primarily been limited to conducting two internal reviews of high-risk medical CDRs, one of which concluded, consistent with the above results, that these CDRs demonstrated no return on investment. Nevertheless, RRB continues to do them. RRB does not routinely compile and analyze data for all of the CDRs it conducts, which limits its ability to identify potential gaps in oversight and to monitor program performance. For example, RRB lacks data that would help it determine how many medical CDRs it should expect to conduct. RRB officials said compiling data can be challenging because it uses multiple data systems. However, by more efficiently collecting and compiling key CDR data, RRB could enhance its capability to routinely assess program performance.
Why GAO Did This Study
RRB is an independent agency that administers disability benefits for railroad workers. In fiscal year 2016, about 31,000 railroad workers with disabilities received $1.1 billion in disability benefits. RRB is generally required to periodically assess beneficiaries' medical condition or earnings through continuing disability reviews (CDRs) to verify that they remain eligible for disability benefits.
This report examines the extent to which RRB (1) conducts medical and earnings CDRs to ensure the continued eligibility of disability beneficiaries, and (2) oversees the CDR program. GAO analyzed data provided by RRB for CDRs completed in fiscal years 2014-2016, the only years for which complete data were available. GAO also reviewed RRB's policies and procedures, a nongeneralizable random sample of 14 CDR cases that were completed in fiscal year 2016, and relevant federal laws and regulations; and interviewed RRB officials.
Recommendations
Congress should consider giving RRB access to the National Directory of New Hires, a national database of wage and employment information that would enable it to identify potential overpayments sooner. GAO is also making three recommendations to RRB, including that it reconsider the purpose and value of high-risk CDRs, and routinely compile and analyze CDR data to improve oversight. RRB agreed with these recommendations.
Matter for Congressional Consideration
| Matter | Status | Comments |
|---|---|---|
| To improve RRB's ability to make accurate disability benefit eligibility determinations, including CDRs, and to decrease the potential for making improper payments, Congress should consider granting RRB access to the Department of Health and Human Services' quarterly earnings information from the National Directory of New Hires database. (Matter for Consideration 1) | As of January 2025, no legislation has been enacted related to this matter to Congress. The Railroad Retirement Board (the Board)'s fiscal year 2020 budget proposal included a legislative proposal to provide the Board no-cost access to the NDNH. However, the Board was denied a free subscription and concluded that access to the NDNH would not be cost-effective. It reported that a subscription to NDNH would cost over $1 million per year, while offsetting about $75,000 in current agency costs. However, NDNH earnings data would provide the Board with more recent earnings data than the agency currently uses for continuing disability reviews and would likely realize savings to the disability trust funds exceeding the additional administrative costs through faster detection of beneficiaries who were no longer eligible for benefits. The Board's analysis did not consider these potential savings to the disability trust funds from reduced overpayments. In April 2024, the Board reported that they requested access to the Social Security Administration's DIB WIZ application, which would provide access to NDNH at no cost to the Board, but as of January 2025 an agency official reported that SSA denied the application. |
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Railroad Retirement Board | To enhance RRB's ability to manage and oversee its CDR program, RRB should develop a standard for the timely processing of disability program overpayments identified through CDRs. (Recommendation 1) |
RRB agreed with this recommendation. As of June 2020, RRB is adding a new internal timeliness objective involving the review and processing of disability cases where a continuing disability review (CDR) is completed by the Disability Benefits Division (DBD) and is referred to the Retirement and Survivor Benefits Division (RSBD) for possible further action, such as suspension, termination, overpayment or underpayment of benefits, as suggested by the CDR. The goal is that RSBD will process 85 percent of completed CDR cases received from the Disability Benefits Division within 120 calendar days of the date assigned. The new timeliness objective is an internal goal added to fiscal year-end customer service goal reporting for RSBD. RRB reached this goal for fiscal years 2018 and 2019; for fiscal year 2020 through May 31, it had processed 72 percent of such CDR cases, in part due to the impact of Covid-19.
|
| Railroad Retirement Board | To enhance RRB's ability to manage and oversee its CDR program, RRB should consider whether to reallocate resources used for high-risk CDRs to other CDR efforts that produce more effective outcomes. (Recommendation 2) |
In August 2018, the Board reported that it concurred with GAO's February 2018 recommendation and ceased allocating resources for high-risk CDRs in April 2018. In fiscal year 2015, the Board began conducting medical CDRs on cases it considered to be at high risk for fraud. It completed 166 of these reviews in fiscal years 2015 and 2016, but none identified any ineligible beneficiaries or overpayments. The high-risk CDR outcomes raised questions about the value and benefit of the Board dedicating resources to conduct these additional reviews. The Board is finalizing its amended policies. Ceasing these reviews will make Board resources available for more productive endeavors.
|
| Railroad Retirement Board | To enhance RRB's ability to manage and oversee its CDR program, RRB should routinely compile and analyze CDR program data, such as the number of cases selected for review, the number of beneficiaries in each medical improvement category, outcomes, and the costs and benefits of conducting CDRs, to improve program oversight. (Recommendation 3) |
RRB agreed with this recommendation. In August 2018, the agency reported that it began reporting in October 2017 weekly pending CDR type action cases to the Director of Programs, and that it had begun tracking CDR reason codes for each medical improvement category. In June 2020, RRB reported that its Program Evaluation and Management Services (PEMS) section will compile and analyze all relevant CDR program case and cost data to better oversee CDRs. In July 2021, RRB said that its first analysis would cover 151 CDR's adjudicated from April 2019 through September 2020. In December 2021, RRB sent the results of its study of CDRs performed during FY 2019 and 2020, which showed counts of CDRs broken out by type, outcome, age, employer, occupation, and other categories. It also showed overpayments uncovered by CDRs and the costs associated with conducting them. RRB said it plans to conduct similar annual CDR reports, issuing the report of the prior FY's CDRs by the end of the following fiscal year.
|
