The Mismatch between Mental Health Care Access and Demand
During hard times, mental health care can be a crucial resource to help with everyday challenges and stresses for people with behavioral health conditions—mental health and substance use disorders. But increasing demand for these services has led to an ongoing, nationwide shortage of behavioral health providers.
Today’s WatchBlog post looks at our work on these shortages, including efforts to increase the number of providers and the effects of shortages on active-duty military servicemembers.
Image

Efforts to increase the number of providers face key barriers
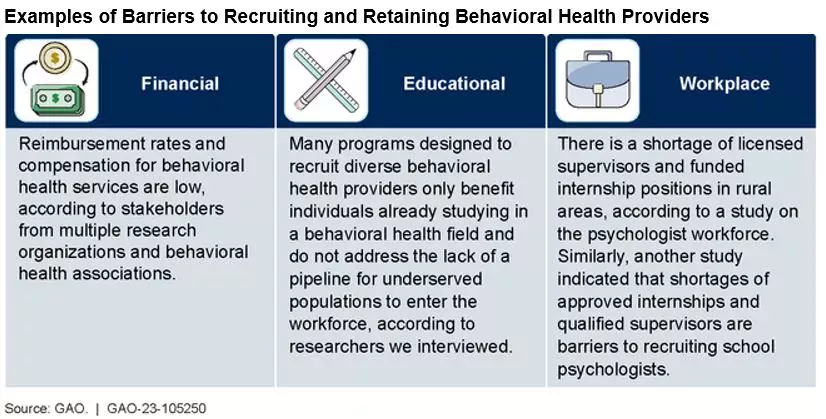
An estimated 53 million adults had a mental illness in 2020. Another 40 million people ages 12 or older (14.5%) had a substance use disorder. But finding a health care provider for these behavioral health issues has proven difficult for many people. In an October 2022 report, we looked at efforts by the Department of Health and Human Services (HHS) to support recruiting and retaining providers. HHS funds education and training programs to help expand the supply and distribution of health care professionals—for example, in underserved or rural areas. But its efforts face several obstacles. For example, in rural areas, there is a shortage of licensed supervisors and funded internship positions to attract new workers, according to one study on the psychologist workforce. Rural behavioral health care providers may also face professional isolation, resource limitations, and long travel distances. These were barriers to retaining and recruiting such providers in rural areas.
More generally, industry stakeholders told us that compensation for behavioral health services is lower than for other forms of medicine. As a result, this health care career path may be less attractive to those, for example, who have large student loan debt.
Stakeholders also told us about a lack of training for providers to serve diverse populations. This has resulted in providers tending to stay in areas where they’ve been trained and serving those populations, leaving some communities without care.
Our October 2022 report details these barriers and HHS’s efforts to address them.
Image
Long wait times for active-duty military
Serving in the military, especially combat, may carry a psychological cost for active-duty service members. If left untreated, behavioral health conditions can worsen with consequences for the service member, as well as for the military.
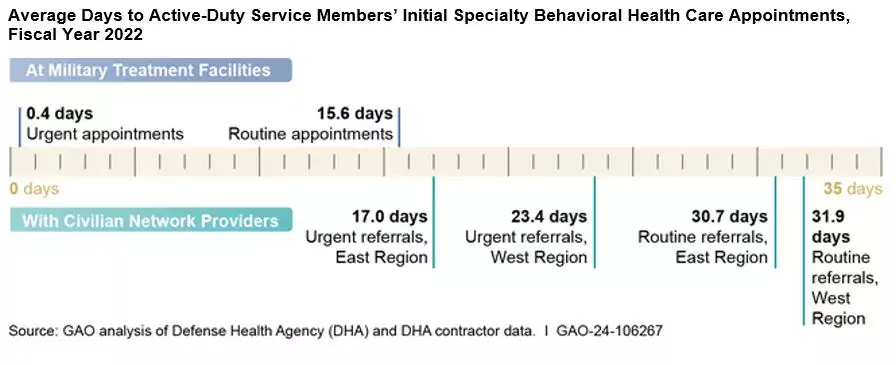
Despite these risks, service members in need of treatment can face long wait times to receive care. For example, when service members were able to receive behavioral health care at military facilities in 2022, they typically could get an initial appointment within just over 2 weeks. But sometimes military facilities can’t accommodate these appointments. When service members were referred to civilian behavioral health care providers, we found that they on average waited a month for initial care. For urgent referrals—where a provider has determined the need for expedited treatment—we found that service members waited on average 2-3 weeks, depending on where they lived.
In our podcast episode with GAO’s Alyssa Hundrup, we discussed these wait times and their impacts. Listen here:
The Department of Defense is taking action to address these wait times. For example, DOD is working to expand the types of providers eligible to provide service members with care, and is testing new approaches, such as increased use of group rather than individual therapy. The department is also expanding the use of telehealth (remote appointments via phone or video conference).
But we think there’s more DOD could do.
We recommended DOD establish a time frame for service members to receive behavior health care appointments specific to urgent referrals to civilian network providers. We also think DOD should regularly monitor the performance of contractors responsible for managing the network providers to ensure they are adhering to those timeframes.
Image
For both the civilian and military communities, ensuring a steady supply of behavioral health providers is essential to making sure that people receive the treatment that they need.
Learn more about our work on mental health topics by checking out our key issue page.
- GAO’s fact-based, nonpartisan information helps Congress and federal agencies improve government. The WatchBlog lets us contextualize GAO’s work a little more for the public. Check out more of our posts at GAO.gov/blog.
GAO Contacts
Related Products

GAO's mission is to provide Congress with fact-based, nonpartisan information that can help improve federal government performance and ensure accountability for the benefit of the American people. GAO launched its WatchBlog in January, 2014, as part of its continuing effort to reach its audiences—Congress and the American people—where they are currently looking for information.
The blog format allows GAO to provide a little more context about its work than it can offer on its other social media platforms. Posts will tie GAO work to current events and the news; show how GAO’s work is affecting agencies or legislation; highlight reports, testimonies, and issue areas where GAO does work; and provide information about GAO itself, among other things.
Please send any feedback on GAO's WatchBlog to blog@gao.gov.