Medicare: Information on the Transition to Alternative Payment Models by Providers in Rural, Health Professional Shortage, or Underserved Areas
Fast Facts
To save money and improve health care quality, Medicare has been trying alternative payment models for reimbursing providers. Some models require providers to use electronic health records or to accept financial risk. That is, providers may receive rewards for meeting care quality goals, but payments could be reduced—or providers could owe money—for falling short.
Fewer providers in rural or provider shortage areas participate in such models. Health associations and others cited barriers to participation. For example, electronic health record systems are expensive, and providers who can't cover potential losses may be more risk averse.
Highlights
What GAO Found
In recent years, the Centers for Medicare & Medicaid Services (CMS) has developed and implemented new Medicare payment models, including alternative payment models (APM), in an effort to shift from paying providers based on the volume of care provided to the quality of care provided (value-based payments). One type of APM, Advanced APMs, are designed to encourage providers to share in both the financial rewards and risk of caring for Medicare beneficiaries. Providers must meet certain requirements to take part in an Advanced APM, such as using certified electronic health record technology.
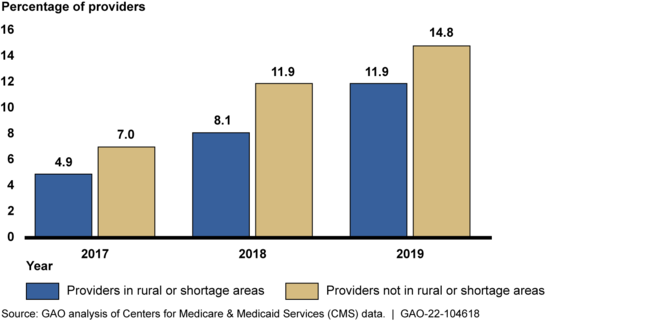
GAO's analysis of CMS data found that a smaller percentage of providers eligible to participate in Advanced APMs (eligible providers) in rural or health professional shortage areas (shortage areas) participated in them each year from 2017 through 2019 compared to providers not located in these areas.
Percentage of Medicare Providers in Rural or Shortage Areas and Providers Not Located in These Areas Who Participated in Advanced APMs, 2017 – 2019
Providers in rural, shortage, or medically underserved areas face financial, technology, and other challenges in transitioning to APMs, including Advanced APMs, according to CMS officials and stakeholders GAO interviewed. These include
- a lack of capital to finance the upfront costs of transitioning to an APM, including purchasing electronic health record technology; and
- challenges acquiring or conducting data analysis necessary for participation.
CMS has implemented models with certain features that may help providers in rural, shortage, or underserved areas transition to APMs, including Advanced APMs. This includes models that offer upfront funding to help with costs associated with participating in the APM, such as hiring additional staff; and technical assistance, such as education about APMs, to support providers.
Why GAO Did This Study
In 2017, in response to the Medicare Access and CHIP Reauthorization Act of 2015, CMS implemented the Quality Payment Program—a payment incentive program intended to reward high-quality, efficient care. Advanced APMs, which offer a 5 percent incentive payment for Medicare providers seeing a certain percentage of their Medicare beneficiaries through the Advanced APM, are one part of this program.
The Medicare Access and CHIP Reauthorization Act of 2015 included a provision for GAO to examine transitions to APMs for providers in rural areas, shortage areas, or medically underserved areas. This report describes (1) participation in Advanced APMs by providers in rural or shortage areas; (2) challenges providers in rural, shortage, or underserved areas face in transitioning to APMs, including Advanced APMs; and (3) actions CMS has taken to help these providers transition to APMs.
GAO analyzed CMS data on participation in Advanced APMs for 2017 through 2019—the most recent years available at the time of GAO's analysis. GAO also interviewed officials from CMS and 18 stakeholder organizations that represent providers of various specialties that participate in APMs or that have conducted research and are knowledgeable of issues related to APMs.
The Department of Health and Human Services provided technical comments on a draft of this report, which GAO incorporated as appropriate.
For more information, contact Michelle B. Rosenberg at (202) 512-7114 or rosenbergm@gao.gov.
