Medicare: CMS Should Provide Beneficiaries More Information about Substance Use Disorder Coverage
Fast Facts
In 2018, almost 5 million Medicare beneficiaries used behavioral health services that the program covers. These include treatments for mental health and substance use disorders.
Medicare wants to expand access to substance use disorder treatment, but some beneficiaries may not know these services are covered. Medicare’s coverage of these treatments is not explicitly outlined in the Medicare & You publication—the most widely disseminated source of information on Medicare coverage for beneficiaries.
We recommended that Medicare include explicit information on covered services for beneficiaries with substance use disorders in this publication.
Medicare Beneficiaries Use of Behavioral Health Services, by Diagnosis Group, 2018
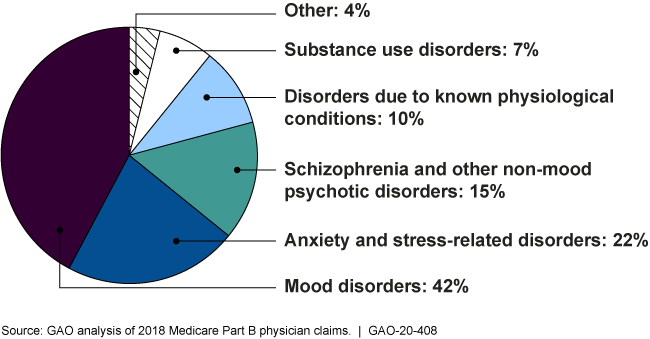
Pie chart
Highlights
What GAO Found
GAO's analysis of Medicare claims data shows that in 2018 almost 5 million beneficiaries used behavioral health services—services for mental and substance use disorders. This represented about 14 percent of the more than 36 million fee-for-service (traditional) Medicare beneficiaries and reflects about $3.3 billion in spending. Additionally, about 96 percent of all behavioral health services accessed by Medicare beneficiaries in 2018, the latest data available, were for a primary diagnosis in one of five behavioral health disorder categories. (See figure.) Mood disorders, such as depression and bipolar disorders, accounted for 42 percent of services. SUD services accounted for about 7 percent of all services accessed by beneficiaries. Further, two-thirds of behavioral health services were provided by psychiatrists, licensed clinical social workers, and psychologists in 2018.
Number of Behavioral Health Services Accessed by Medicare Beneficiaries, by Diagnosis Group, 2018

The Centers for Medicare & Medicaid Services (CMS), the Department of Health and Human Services' (HHS) agency that administers Medicare, uses various approaches to disseminate information to Medicare beneficiaries about coverage for behavioral health services. As part of these efforts, CMS mails out Medicare & You —the most widely disseminated source of information on Medicare benefits—to all Medicare beneficiaries every year. GAO reviewed the fall 2019 and January 2020 editions of Medicare & You. While the January 2020 edition describes a new coverage benefit for beneficiaries with opioid use disorders, neither edition includes an explicit and broader description of the covered services available for substance use disorders. Both HHS and CMS have stated that addressing substance use disorders is a top priority. Given that coverage for substance use disorders is not explicitly outlined in Medicare's most widely disseminated communication, Medicare beneficiaries may be unaware of this coverage and may not seek needed treatment as a result.
Why GAO Did This Study
Behavioral health disorders often go untreated, potentially leading to negative health consequences. Behavioral health disorders include substance use or mental health disorders. Medicare provides coverage for behavioral health services. The Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act enacted in 2018 included a provision for GAO to examine Medicare behavioral health services and how beneficiaries are informed of coverage and treatment options.
This report (1) describes the utilization of behavioral health services by Medicare beneficiaries and the types of providers furnishing these services, and (2) examines how CMS provides information to beneficiaries about their coverage for behavioral health services. To describe service utilization and provider types, GAO analyzed 2018 Medicare claims data, the most recent data available. To examine how CMS shares information with beneficiaries, GAO reviewed CMS requirements for providing coverage information to beneficiaries, reviewed CMS publications, and interviewed CMS officials.
Recommendations
CMS should include explicit information on the services covered by Medicare for beneficiaries with substance use disorder in its Medicare & You publication. HHS reviewed a draft of this report and concurred with the recommendation.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should ensure that the Medicare & You publication includes explicit information on the services covered by the Medicare program for beneficiaries with a SUD. (Recommendation 1) |
Closed – Implemented
HHS concurred with this recommendation. CMS updated the September 2020 version of the "Medicare & You" handbook to include explicit information on the services covered by the Medicare program for beneficiaries with substance use disorders. According to CMS, the handbook was distributed to every beneficiary's household and posted on Medicare.gov in late September 2020. As such, we are closing the recommendation as implemented.
|
