Medicare Provider Education: Oversight of Efforts to Reduce Improper Billing Needs Improvement
Fast Facts
In 2016, Medicare's fee-for-service program made $41.1 billion in improper payments. To help ensure that payments are made properly, the Centers for Medicare & Medicaid Services contracts with Medicare Administrative Contractors (MACs) to educate health care providers.
We reviewed these contractors and found issues with CMS's requirements and oversight of them. For example, MACs are not required to educate some providers about proper billing for certain services with high improper payment rates. We recommended that CMS require MACs to educate these providers and establish metrics to determine if certain MAC reviews help reduce billing errors.
Improper Payment Rates for Overall Medicare Fee-for-Service, Durable Medical Equipment, Prosthetics, Orthotics, and Supplies and Home Health Services for Fiscal Years 2010-2016
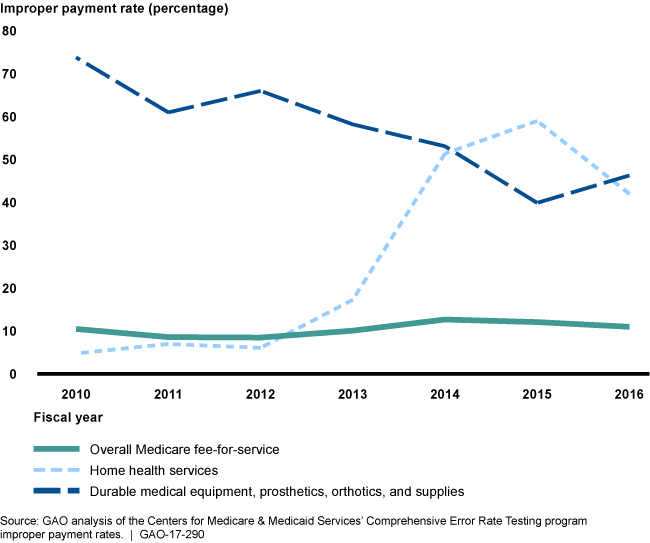
Line graphs showing trends in improper payment rates with fee-for-service being the lowest overall.
Highlights
What GAO Found
Medicare administrative contractors (MAC) process Medicare claims, identify areas vulnerable to improper billing, and develop general education efforts focused on these areas. MAC officials state that their provider education departments focus their educational efforts on areas vulnerable to improper billing; however, the Centers for Medicare & Medicaid Services' (CMS)--the agency within the Department of Health and Human Services (HHS) that administers Medicare--oversight and requirements for these efforts are limited.
- CMS collects limited information about how these efforts focus on the areas MACs identify as vulnerable to improper billing. According to CMS officials, the agency has not required the MACs to provide specifics on their provider education department efforts in these reports because it does not want to be overly prescriptive regarding MAC provider education department efforts. Federal internal control standards state that management should use quality reporting information to achieve the entity's objectives. Unless CMS requires sufficient MAC provider education department reporting, it cannot ensure that the departments' efforts are focused on areas vulnerable to improper billing.
- CMS does not require MACs to educate providers who refer patients for durable medical equipment (DME), including prosthetics, orthotics, and supplies, and home health services on proper billing documentation, nor does it explicitly require MACs to work together to provide this education. HHS has reported that a large portion of the high improper payment rates in these services is related to insufficient documentation. The absence of a requirement for MACs to educate referring providers about proper documentation for DME and home health claims is inconsistent with federal internal control standards, which state that in order to achieve an entity's objectives, management should assign responsibility and delegate authority. Without an explicit requirement from CMS to educate these referring providers, billing errors due to insufficient documentation may persist.
Short-stay hospital and home health claims have been the focus of the MACs' probe and educate reviews--a CMS strategy to help providers improve billing in certain areas vulnerable to improper billing. Under the probe and educate reviews, MACs review a sample of claims from every provider and then offer individualized education to reduce billing errors. CMS officials consider the completed short-stay hospital reviews to be a success based on anecdotal feedback from providers. However, the effectiveness of these reviews cannot be confirmed because CMS did not establish performance metrics to determine whether the reviews were effective in reducing improper billing. Furthermore, GAO found the percentage of claims remained high throughout the three rounds of the review process, despite the offer of education after each round. Federal internal control standards state that management should define objectives in specific and measurable terms and evaluate results against those objectives. Without performance metrics, CMS cannot determine whether future probe and educate reviews would be effective in reducing improper billing.
Why GAO Did This Study
For fiscal year 2016, HHS reported an estimated 11 percent improper payment rate and $41.1 billion in improper payments in the Medicare fee-for-service program. To help ensure payments are made properly, CMS contracts with MACs to conduct provider education efforts. CMS cites the MACs’ provider education department efforts as an important way to reduce improper payments.
GAO was asked to examine MACs’ provider education department efforts and the results of MACs’ probe and educate reviews. This report examines (1) the focus of MACs’ provider education department efforts to help reduce improper billing and CMS oversight of these efforts and (2) the extent to which CMS measured the effectiveness of the MAC probe and educate reviews. GAO reviewed and analyzed CMS and MAC documents and MAC probe and educate review data for 2013-2016; interviewed CMS and MAC officials; and assessed CMS’s oversight activities against federal internal control standards
Recommendations
GAO recommends that CMS should (1) require sufficient detail in MAC reporting to determine the extent to which MACs' provider education department efforts focus on vulnerable areas, (2) explicitly require MACs to work together to educate referring providers on proper documentation for DME and home health services, and (3) establish performance metrics for future probe and educate reviews. HHS concurred with GAO's recommendations.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Centers for Medicare & Medicaid Services | To ensure MACs' provider education efforts are focused on areas vulnerable to improper billing and to strengthen CMS's oversight of those efforts, CMS should require sufficient detail in MAC reporting to allow CMS to determine the extent to which MACs' provider education department efforts focus on areas identified as vulnerable to improper billing. |
HHS concurred with this recommendation and said it would take steps to implement it. In April 2017, CMS released a revised Provider Customer Service Program Activity Report (PAR) template to Medicare Administrative Contractors (MAC). This revised template collects information from MACs on which of their provider outreach and education activities are geared towards the prioritized problem areas identified in their Improper Payment Reduction Strategies. It asks MACs to describe the frequency of education and how it was delivered and if the education was directed primarily at providers who had the highest rate of improper payment, those who had the greatest dollar amount of improper payments, or both. All PAR Reports submitted after July 2017 include this information.
|
| Centers for Medicare & Medicaid Services | To ensure MACs' provider education efforts are focused on areas vulnerable to improper billing and to strengthen CMS's oversight of those efforts, CMS should explicitly require that Medicare Part A and B claims, DME, and home health and hospice MACs work together to educate referring providers on documentation requirements for DME and home health services. |
HHS concurred with this recommendation and said it would take steps to implement it. As of November 2017, CMS within HHS added new language to Internet Only Manual (IOM) Pub 100-9, Chapter 6 requiring MACs to work together to educate providers. Specifically, the language states that MACs are tasked with collaborating with other MACs to educate ordering or referring providers on such things as documentation requirements for items or services, such as orders or referrals for tests, imaging procedures, durable medical equipment, prosthetics, orthotics and supplies (DMEPOS), and home health services especially when the ordering or referring provider is in a different MAC jurisdiction than the servicing provider.
|
| Centers for Medicare & Medicaid Services | To ensure MACs' provider education efforts are focused on areas vulnerable to improper billing and to strengthen CMS's oversight of those efforts, for any future probe and educate reviews, CMS should establish performance metrics that will help the agency determine the reviews' effectiveness in reducing improper billing. |
HHS concurred with this recommendation and said it would take steps to implement it. In October 2017, CMS expanded the Targeted Probe and Educate (TPE) Pilot across all MACs via Change Request (CR) 10249. CR 10249 included a template of MAC monthly reporting metrics for CMS to monitor the outcome and impact of the TPE reviews.
|
