Medicaid Managed Care: Trends in Federal Spending and State Oversight of Costs and Enrollment
Highlights
What GAO Found
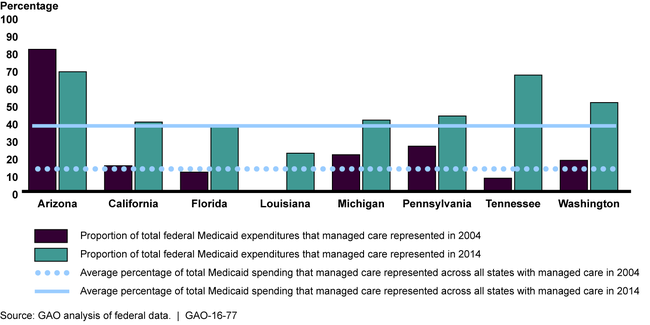
Federal spending for Medicaid managed care increased significantly from fiscal year 2004 through fiscal year 2014 (from $27 billion to $107 billion), and represented 38 percent of total federal Medicaid spending in fiscal year 2014. Consistent with this national trend, managed care as a proportion of total federal Medicaid spending was higher in seven of eight selected states in fiscal year 2014 compared with fiscal year 2004.
Federal Expenditures for Medicaid Managed Care as a Percentage of Federal Medicaid Expenditures, in Eight States, Fiscal Years 2004 and 2014
Total and average per beneficiary payments by states to managed care organizations (MCOs) varied considerably across the eight selected states in state fiscal year 2014. For example, total payments ranged from $1.3 billion in one state to $18.2 billion in another, and average payments per beneficiary ranged from about $2,800 to about $5,200.
While not required by federal policy to do so, five of the eight selected states required MCOs to annually meet minimum medical loss ratio (MLR) percentages—standards that ensure a certain proportion of payments are for medical care and, in effect, limit the amount that can be used for administrative cost and profit. These state minimums generally ranged from 83 to 85 percent, similar to the 85 percent minimums established in the Patient Protection and Affordable Care Act (PPACA) for other sources of health coverage. All MCOs in the five states had MLRs in state fiscal year 2014 that were above the state-required minimums.
GAO also found that all eight selected states focused on beneficiary factors, such as assigning a beneficiary to the same managed care plan in which a family member is enrolled, when the state selects a plan for the beneficiary in the absence of the beneficiary choosing a plan—referred to as auto assignment. States also considered plan performance, for example, on quality measures and program goals, such as achieving a certain distribution of enrollment across plans. Auto assignments of beneficiaries ranged from 23 to 61 percent of managed care enrollees across the seven selected states that tracked such data.
Why GAO Did This Study
The importance of managed care in Medicaid—under which states contract with MCOs to provide a specific set of services—has increased as states expand eligibility for Medicaid under PPACA and increasingly move populations with complex health needs into managed care. States have flexibility within broad federal parameters to design and implement their Medicaid programs, and therefore play a critical role in overseeing managed care. GAO was asked to examine managed care expenditures and provide information on certain components of state oversight of Medicaid managed care.
In this report, GAO analyzes (1) federal expenditures for Medicaid managed care and the range in selected states' payments made to MCOs; (2) selected states' MLR standards and how they compare with federal standards for other sources of health coverage; and (3) selected states' methods for automatically assigning Medicaid beneficiaries to MCO plans. GAO analyzed federal data on Medicaid expenditures for comprehensive risk-based managed care. GAO selected eight states because they used managed care for some portion of their Medicaid population and were geographically diverse. For these states, GAO reviewed state payment data and documentation, including contracts with MCOs, and interviewed state officials. GAO also reviewed federal laws to describe MLR minimums in Medicare and the private insurance market.
The Department of Health and Human Services had no comments on this report.
For more information, contact Carolyn L. Yocom at (202) 512-7114 or yocomc@gao.gov.
