Medicaid Payment: Comparisons of Selected Services under Fee-for-Service, Managed Care, and Private Insurance
Highlights
What GAO Found
Payments to physicians under Medicaid fee-for-service (FFS) and managed care for the 26 evaluation and management (E/M) services, such as office visits and emergency care, that GAO reviewed were generally lower than private insurance prior to the temporary increases mandated by the Health Care and Education Reconciliation Act of 2010 (HCERA). Specifically, in the 40 states where GAO compared Medicaid FFS payments to private insurance, FFS payments were 27 to 65 percent lower than private insurance in 31 states; and in the 23 states where GAO compared managed care payments to private insurance, managed care payments were 31 to 65 percent lower than private insurance in 18 states. Among the three types of E/M services analyzed (office visits, hospital care, and emergency care), Medicaid payments generally were lower than private insurance for all three types, but the magnitude of the difference was often largest for emergency care and smallest for office visits.
Within the Medicaid program, managed care payments for E/M services were generally equal to or higher than FFS prior to the HCERA-mandated increases. Specifically, in the 20 states where GAO compared managed care payments to FFS, managed care payments were 0 to 12 percent higher than FFS in 15 states. Managed care payments for emergency care and hospital care were approximately equal to FFS payments in most states, while office visits showed more variation.
Medicaid Managed Care Payments for Evaluation and Management Services Relative to Medicaid Fee-for-Service in Selected States
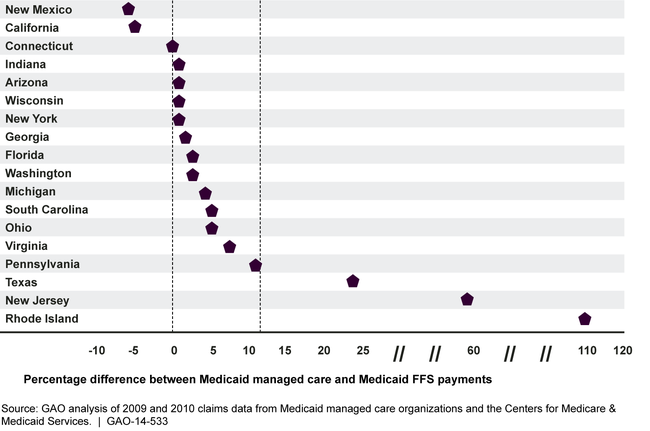
Note: To safeguard confidential information, results were excluded from the figure for 2 of the 20 selected states where the number of Medicaid managed care organizations was limited.
Why GAO Did This Study
Medicaid provided health coverage for over 70 million individuals in fiscal year 2013 through a combination of FFS and managed care at a cost of about $460 billion. Yet, limited information is available on how provider payments per service under Medicaid FFS and managed care compare with private insurance and with one another. This report builds on a prior GAO study on Medicaid payments by comparing payments for E/M services under Medicaid FFS, managed care, and private insurance prior to 2013, when temporary Medicaid payment increases for these services took effect, as mandated by HCERA.
In this report, GAO examines: (1) how payments for E/M services under Medicaid FFS and Medicaid managed care compared with private health insurance prior to the HCERA-mandated increases; and (2) how payments for E/M services under Medicaid managed care compared with Medicaid FFS prior to the HCERA-mandated increases.
To compare these payments, GAO analyzed claims data from Medicaid FFS, managed care organizations, and private insurers. GAO compared payments to physicians for 26 E/M services in selected states, chosen on the basis of data availability. GAO compared Medicaid FFS payments with private insurance in 40 states; Medicaid managed care with private insurance in 23 states; and Medicaid managed care with Medicaid FFS in 20 states. Results were based primarily on 2010 data—the most recent Medicaid FFS data available for most states—but 2009 data were used when 2010 data were unavailable.
For more information, contact Carolyn L. Yocom at (202) 512-7114 or yocomc@gao.gov.
